In this paper Tiegs-Heiden et al. describe the findings of an entity (lumbar painful lipoma also named back mice) that the radiologist can encounter in musculoskeletal ultrasound practices, so they should be aware of it. Patients are usually referred by what the physician thought that could be a painful lipoma. But the sonographic features of this lumbar nodule or mass ARE NOT of a lipoma and should be described as back mouse/mice or subfascial fat herniation (despite no clear trans-fascial herniation is visualized, it is suggested by its mobility sliding beneath the superficial fascial layer).
Notes on the article of:
Tiegs-Heiden C. A., Murthy N. S., Glazebrook K. N., Skinner J. A.
Subfascial fat herniation: sonographic features of back mice.
Skeletal Radiol. 2017 Sep 15. doi: 10.1007/s00256-017-2772-9. PubMed PMID: 28914351.
About what is known of the entity back mice
-Tiegs-Heiden et al. state that “back mice” (painful lipoma) are an uncommon cause of lumbar mass and/or low back pain. There is variability in the reported prevalence, and they seem to be more common in females. The group of Tiegs-Heiden et al. mention that the back mice haven’t been previously reported in the radiology literature as far as they know.
-They comment the different names it has in the medical literature (episacral lipoma, subfascial fat herniation, fibro-fatty nodule, and fibrositis).
-They described them as round or oval lesions near the posterior superior iliac spine.
-They clarify that back mice is a distinct entity from a hernia of the Petit’s inferior lumbar triangle (Light 1983).
-Patients report a painful, somewhat mobile, rubbery subcutaneous nodule/mass in the lumbosacral region (usually is reported as painful lipoma). Often located near the sacroiliac “dimple” (Singewald 1966). Pain can radiate, and can be chronic or acute.
-Treatment can include injection with local anesthetic and corticoesteroid or surgical resection.
Sonographic features of 3 case stories, all 3 referred from the physician as suspicious of painful lipoma
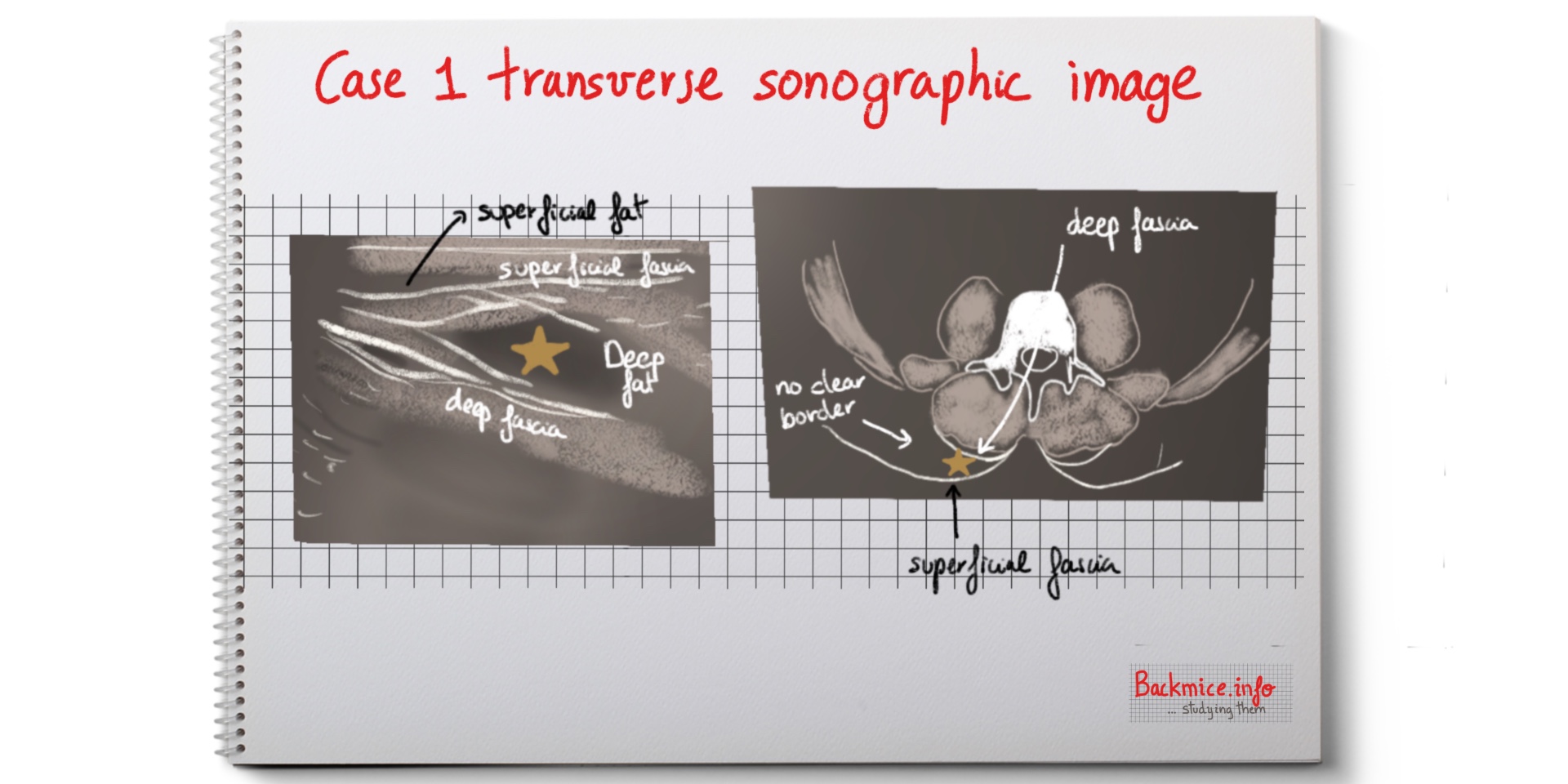
Case 1: a 65-year-old male with a painful mass in right lumbar region. At least present for 4 months. No trauma history. Described as dull ache. Clinical examination showed a mobile mass 3-4 cm right from midline in the low back.
Sonographic examination demonstrated a 3.4×3.1×1 of fat located between the superficial and deep fascial planes, near the posterior superior iliac spine. The lateral border was not discernible. No increased Doppler imaging. The mass had mobility between the fascial planes. There was symmetric lesion on the left but not mobile.
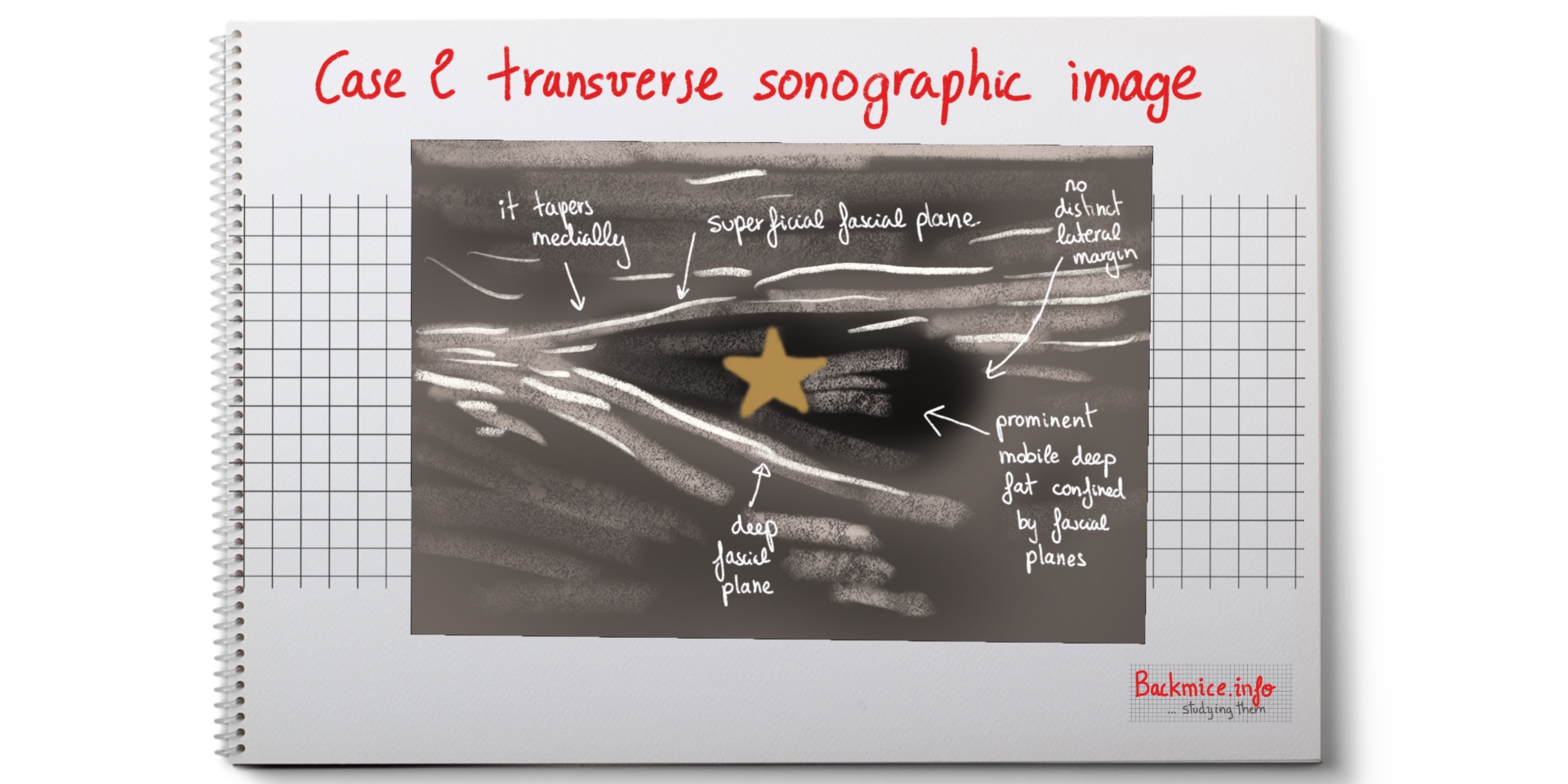
Case 2: a 47-year-old female who presented a palpable mass in the right low back and intermittent back pain for at least a year (the pain usually lasting about a week and then remitting). Clinical examination showed a 4-5 cm subcutaneous mass in the posterior superior spine surface. It felt like a lipoma.
Ultrasound demonstrated that it correlated to deep fat between the superficial and deep fascial planes (area 4.5×2.7×1.1). Confined by fascial planes (laterally there was no discrete border). Mobile on dynamic examination especially in medial border. Medial border was tapered. Doppler showed no hyperaemia.
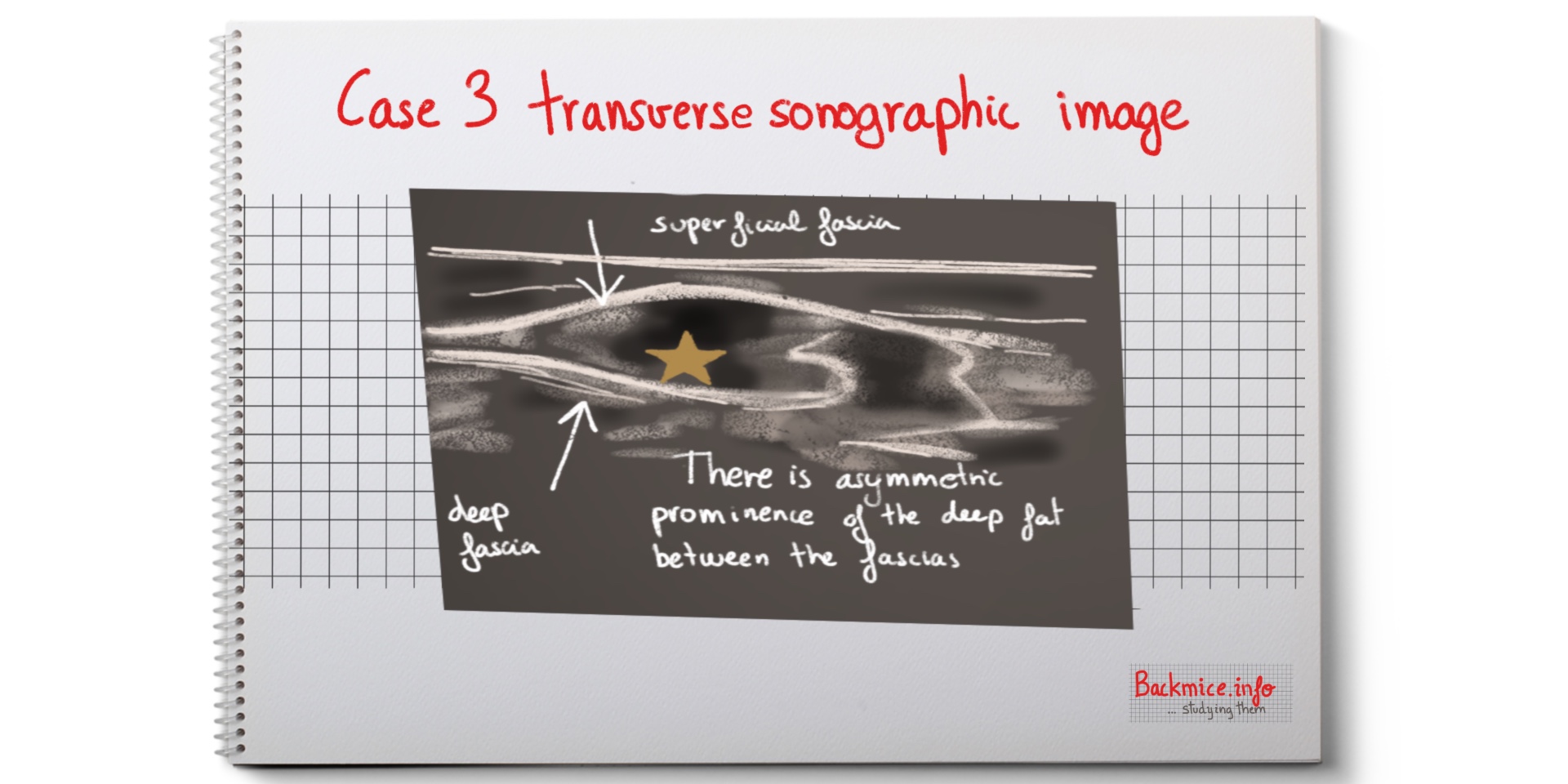
Case 3: a 42-year-old female presented with a painful mass which she noticed 1 week prior. No history of trauma. Clinical examination showed 2.5 cm oblong subcutaneous nodule in the right lumbosacral region. It was tender to the touch. The clinician noted a “tail-like” tapering projection along the medial margin. The clinician thought it could be a lipoma.
Ultrasound demonstrated asymmetric prominence of the deep subcutaneous fat on the right. There was no lateral border. The subcutaneous fascial planes confined it. It was tender to the touch.
Notes about the discussion: “mobility matters”
They report 3 cases of back mice, defined as mobile subcutaneous mass in the lumbosacral region that is often painful. Regardless in the literature they are also described as trans-fascial herniation.
The patients in this study presented a palpable mass corresponded to fat between superficial and deep fascia layers. Two patients described it as a painful mass.
-In all cases fat was incompletely encapsulated, with NO DISCERNIBLE BORDER ON ITS LATERAL MARGIN.
-The location was just off midline near the posterior superior iliac spine.
-In all cases fat was bilateral; nevertheless, it was mobile in the symptomatic side and immobile in the asymptomatic side.
-NO case of herniation though a fascial defect.
-This mobility is responsible for the clinical presentation of back mice. The fat abnormally moves, sliding beneath the superficial fascial layer in the painful side. And it is immobile in the asymptomatic side.
-Tiegs-Heiden et al. prefer the terms “subfascial fat herniation” or back mouse, and not “episacral lipoma” since there is not capsule.
The sonographic features reported of back mice suggest that: hypermobile deep fat mass between the superficial and the deep fascial layers in the low back is not encapsulated laterally.
References
- Curtis P, Gibbons G, Price J. Fibro-fatty nodules and low back pain: the back mouse masquerade. J Fam Pract. 2000;49(4):345–8.
- Motyka TM, Howes BR, Gwyther RE, Curtis P. Treatment of low back pain associated with Bback mice^: a case series. J Clin Rheumatol. 2000;6(3):136–41.
- Singewald ML. Another cause of low back pain: lipomata in the sacroiliac region. Trans Am Clin Climatol Assoc. 1966;77:73–9.
- Wollgast GF, Afeman CE. Sacroiliac (episacral) lipomas. Arch Surg. 1961;83:925–7.
- Erdem HR, Nacir B, Ozeri Z, Karagoz A. Episacral lipoma: a treat- able cause of low back pain. Agri Derg. 2013;25(2):83–6.
- Herz R. Subfascial fat herniation as a cause of low back pain: differential diagnosis and incidence in 302 cases of backache. Ann Rheum Dis. 1952;11(1):30–5.
- Light HG. Hernia of the inferior lumbar space: a cause of back pain. Arch Surg. 1983;118(9):1077–80.
- Bicket MC, Simmons C, Zheng Y. The best-laid plans of Bback mice^ and men: a case report and literature review of episacroiliac lipoma. Pain Physician. 2016;19(3):181–8.
- Copeman WS. Fibro-fatty tissue and its relation to certain rheumat- ic syndromes. Br Med J. 1949;2(4620):191–7.
- Curtis P. In search of the ‘back mouse’. J Fam Pract. 1993;36(6): 657–9.