(webpage under construction as our research progresses)
Last updated: the information you are currently reading is not updated as of January 2024.
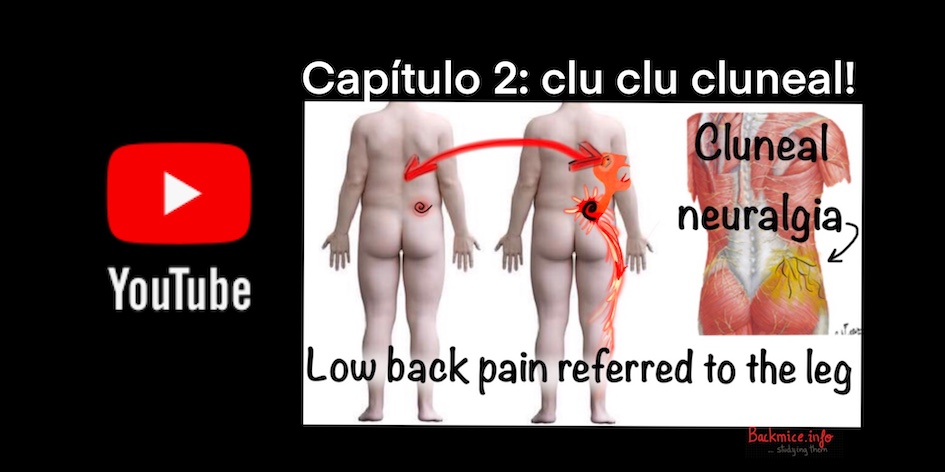
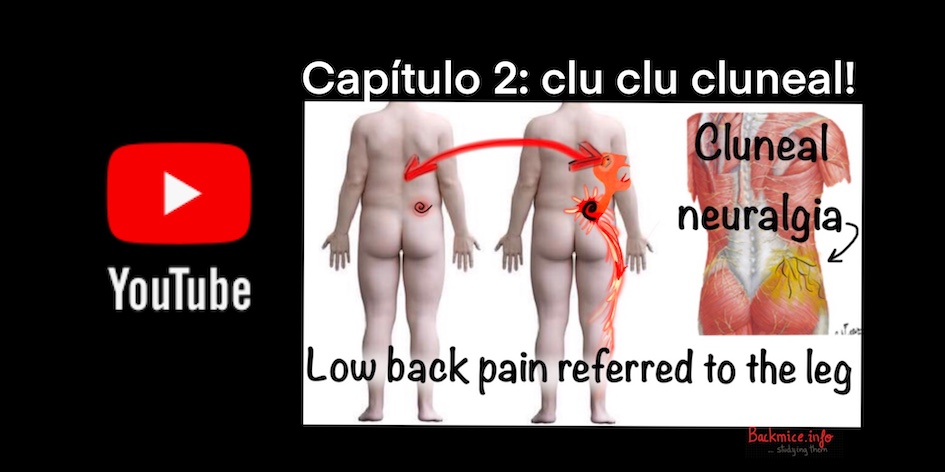
(First, please check our video posted in October 2023 on "Cluneal nerve entrapment" and the "back mice phenomenon")
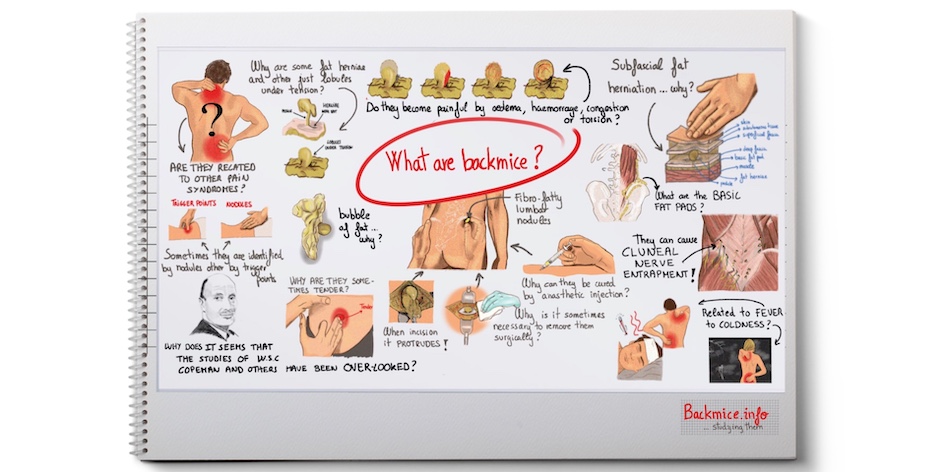
Important note: This website is dedicated to exploring the subject of ‘fibro-fatty lumbar nodules’, which are known by various names such as ‘back mice or back mouse’, ‘episacral or episacroiliac lipoma’, ‘subfascial fat herniations’, and ‘Copeman’s nodules’… among others. To ensure uniformity across the website, the term ‘back mice’, coined by Peter Curtis in the 1990s, will be consistently utilized.
NOTE: In 2023, we began conducting human cadaveric dissections with the aim of gaining a better understanding of the ‘back mice phenomenon.’ These observations can be summarized on our YouTube Channel, which has led us to preliminary conclusions that may provide new insights into the ‘back mice conundrum.’ → LINK to the YouTube videos related to the findings from our cadaveric human dissections.
Welcome to the webpage www.backmice.info!
The website is authored by Marta Cañis Parera, a medical doctor and researcher specializing in ‘back mice’ and fibro-fatty tissue dysfunction (now referred to as fascia dysfunction) as a potential cause of low back pain. She also explores related issues such as cluneal nerve entrapment, pain mechanisms, and the underlying structure of fibrofatty tissue.
Established in March 2018 as part of an ongoing research project initiated in the summer of 2017, the website is regularly updated with the latest information as the research progresses.
The webpage’s design emulates a researcher’s notebook, fostering an atmosphere of exploration and ongoing investigation.
It’s important to understand that the information provided on the website represents the researcher’s questions, findings, theories, and perspectives, and should be interpreted within the context of ongoing research. The main objective of the webpage is to provide an answer to the question “What are ‘back mice’?” and explore all the relevant clinical entities associated with them.
Our Spanish research team consists of Marta Expósito Izquierdo and myself, both of whom are medical doctors in the final stages of our medical PhD program. We are working under the guidance of our thesis director, Dr. Juan Jose Cabre Vila.
→LINK to access the page where you can view our curriculum backgrounds
“We hope that other researchers, health professionals and patients will find this site interesting and valuable.”
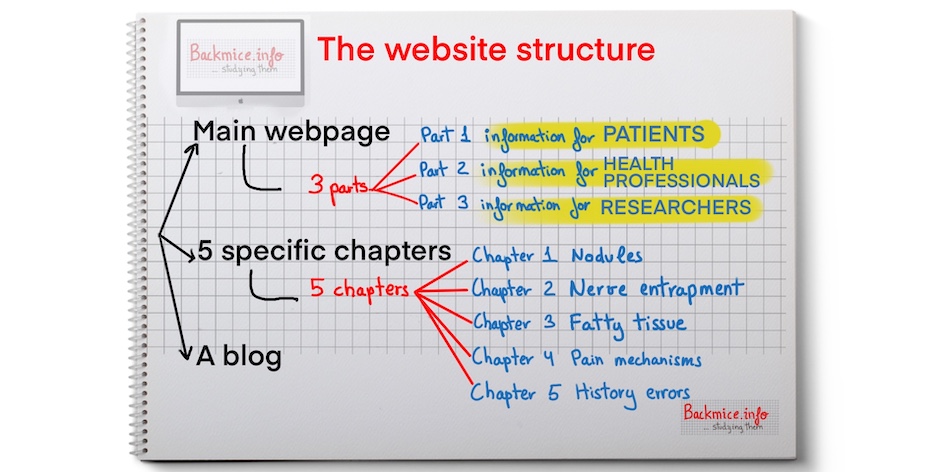
The structure of the website backmice.info and its goal:
The website backmice.info is structured to provide comprehensive information about back mice. It consists of a main webpage with three sections catering to patients, health professionals, and researchers. Additionally, there are five in-depth chapters covering various aspects related to back mice, such as painful nodules, peripheral nerve entrapments, fatty tissue, pain mechanisms, and historical errors. The website also features a blog where contributions from patients, health professionals, and researchers are encouraged.
Our main objective is to facilitate the sharing of information and research on ‘back mice’ among researchers, health professionals, and interested individuals. To achieve this, we have developed a comprehensive website and two dedicated YouTube channels.
- →LINK to YouTube Channel: BACK MICE
- →LINK to Youtube Channel: DIARIO DE UNA INVESTIGADORA SIN GLAMOUR (English subtitles)
Through these platforms, we aim to bridge the gap between research and practical application by providing clear and accessible content.
Our interest in the backmice.info project is entirely altruistic, as we firmly believe in the importance of sharing knowledge.
Shedding light on the frequently overlooked and under-diagnosed cause of low back pain in specific patients, ‘back mice’, is of utmost importance for us.
If you have any contributions, corrections, or remarks, or if you simply wish to get in touch, please feel free to email us at:
We deeply value your engagement and eagerly look forward to hearing from you.
PART 1: Useful Information for PATIENTS
If you are a patient conducting your own research on the topic of ‘back mice’, there are a few important things you should know: we do not offer medical diagnosis or treatment for the medical condition being studied on this website. Our current focus is on conducting investigations and providing comprehensive information about the condition.
Nevertheless, If you believe you are a back mice patient, though we are unable to offer medical assistance or treatment directly, we provide additional guidance on this webpage regarding how you can seek medical assistance from your healthcare professionals.
“We believe in patient empowerment”
Patient guidance for requesting a medical assessment without being dismissed:
- Part 1.1 – The first step “a willing to listen doctor”
- Part 1.2 – The Palpation Technique
- Part 1.3 – The Medical Terminology
- Part 1.4 – The Diagnostic Imagining
- Part 1.5 – Pain Relief
- Part 1.6 – Considering surgery
As we mentioned, the topic of painful and non-painful ‘back mice’ or subfascial fat herniations and their relation to low back pain is definitely overlooked by mainstream medicine today.
While we are actively engaged in efforts to rectify this situation, it is important to acknowledge that during your visits to doctors or other healthcare professionals, they may not be well-versed in this specific condition. In fact, our own team only became aware of this condition in 2017. To assist you in navigating this challenge, we offer guidance on the optimal approach for seeking medical diagnosis and assessment.
Part 1.1 – The first step: a “willing to listen” physician (Patient Guidance)
First step is to find a “willing to listen doctor”: The most common scenario is when your doctor is not familiar with the existence of ‘back mice’. Consequently, it is understandable that they may react in a perplexing way when you ask them to follow the recommendations provided in this guidance. However, with effective communication skills, progress can be made. That’s why it is important to familiarize them with this medical entity by following our guidance.
Part 1.2 – What is your case? Painful or non-painful (Patient Guidance)
There are two primary categories of patients who typically search for information about back mice on the internet:
- Patients with non-painful ‘back mice’: This group often discovers the deep fibrofatty nodule accidentally while soaping their low back, applying cream, or receiving massages. Despite not experiencing pain, these patients may seek information for two main reasons: curiosity and concern about the possibility of cancer. For this group, consulting a doctor is recommended. A medical professional can provide a diagnosis of a benign palpating-like nodule and, if necessary, may supplement the diagnosis with an ultrasound, especially for patients who are worried.
- Patients with painful ‘back mice’: Assisting patients who suffer from pain caused by ‘back mice’ is our main concern. Our research has provided us with knowledge that can help alleviate their pain to some extent.
- The main recommendations are:
- Find a doctor who is willing to listen to your concerns.
- Assist the doctor in locating the deep fibrofatty nodule through palpation.
- Request an ultrasound to aid in the diagnosis.
- Discuss pain relief options with your doctor.
- The main recommendations are:
Part 1.3 – The palpation technique (Patient Guidance)
Assist your doctor in effectively palpating the nodule using the most appropriate technique. Assist your doctor in effectively identifying the nodule by describing its location in the lumbar region.
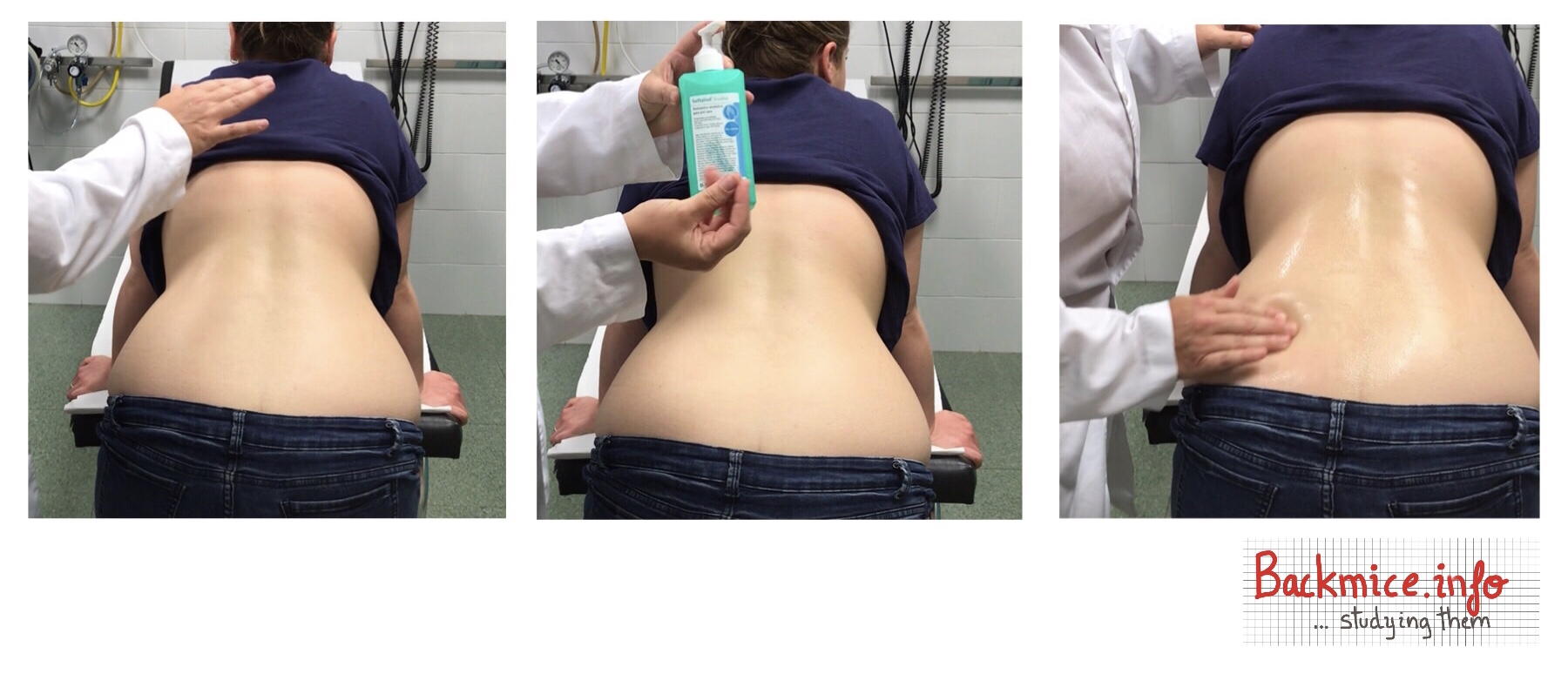
PALPATION TECHNIQUE: It is crucial to let your doctor feel the nodule while you are standing, using a lubricant like hydroalcoholic gel to facilitate palpation. If your doctor examines you with dry rubber gloves, they may have difficulty feeling the nodule as fingers require lubrication. Furthermore, ensure that you are standing with your back slightly inclined during the examination to ensure accurate assessment and prevent the possibility of missing the presence of the deep nodule. →Link to a YouTube video demonstrating the proper technique for palpation.
Part 1.4 – The medical terms (Patient Guidance)
Present medical terminology and provide relevant medical literature to your doctor. Use the term “episacroiliac lipoma” or “subfascial fat herniation” instead of “back mouse” as it carries a more serious and medically recognized connotation.
To support your request, we recommend referring to relevant PubMed abstracts (You can also print them out to show to your doctor) from recent medical articles on subfascial fat herniation or back mouse. These abstracts will demonstrate that your information is derived from reliable scientific sources. It is important to understand that healthcare professionals may initially exhibit hesitancy towards concepts that have not yet been extensively taught in medical universities or discussed in major medical conferences. The idea that something palpable can remain relatively unknown can be perplexing and even surreal for doctors. LINK TO ABSTRACTS:
→Subfascial fat herniation: sonographic features of back mice. Published in 2017 by a team of the Mayo Clinic
→The Best-Laid Plans of “Back Mice” and Men: A Case Report and Literature Review of Episacroiliac Lipoma. Published in 2016.
→Historical Review of Studies on Sacroiliac Fatty Nodules (Recently Termed “Back Mice”) as a Potential Cause of Low Back Pain. Published in 2021
Part 1.5 – Diagnostic imaging (Patient Guidance)
Request an ultrasound examination to confirm that de deep nodule is due to “episacral lipoma or subfascial fat herniation”.
This imaging test can provide valuable diagnostic information. In certain cases, an MRI may complement the ultrasound examination. You can refer your doctor to a radiology page that shows a case of a back mouse. →Here is a LINK to the radiology page Episacral lipoma – “Back mouse”, Radiopaedia.org
Part 1.6 – Pain relief (Patient guidance)
In case of painful back mice, ask for pain relief. If the nodules cause pain upon palpation and lead to low back pain or referred pain to the leg, it is advisable to request a diagnostic test utilizing local anesthetic blockade. This procedure involves injecting a small amount (1-2ml) of local anesthetic, provided it is not contraindicated for you, using a short needle (no longer than 1.6mm) around and within the nodule. By performing this procedure, a superior cluneal nerve blockade can be achieved, effectively blocking the local small nerves. This serves both as a diagnostic test to determine if the pain originates from that area and as a therapeutic measure. → Link to a video of a local anesthetic block of simple back mouse.
If the pain temporarily subsides but returns after some time (hours or days), it is possible to repeat the technique using multiple dry needling or local anesthetic injections beneath the skin. Dry needling can be conducted using a 30G needle (0.3mm x 8mm) multiple times in each hyperalgesic spot of the affected area. This technique can be performed and repeated within a few days to manage the pain. It is important to note that bruising or discoloration (equimosis) may occur as a result of this technique.
Part 1.7 – Considering surgery (Patient Guidance)
If the pain continues to recur, surgery could be considered. However, it’s crucial to ensure that the surgeon performing the surgery is familiar with this topic and knowledgeable about superior cluneal nerve entrapment issues.
Furthermore, you can explore the comments section on our blog entries and YouTube channel to read about other patients’ experiences.
→LINK to access the comments on our blog
→LINK to access the comments to our YouTube Channel BACK MICE
→LINK to the Youtube video of Hilma Volk: Lumps in Low Back, Top of Hip
Further information for patients:
→LINK To my YouTube Video: This is a 27-minute-long video that aims to explain in the clearest and most amusing YouTuber-style manner why back mice could cause superior cluneal nerve entrapment. Additionally, it explains why this cluneal neuralgia creates low back pain that can refer down to the leg. Although it is in Spanish, it has English subtitles.
→ LINK to my YouTube Video: This is a 5-minute-long video, the first in a series, where I attempt to explain the reasons behind back mice or Copeman’s nodules (another name for lumbar fibrofatty nodules) being overlooked by mainstream medicine nowadays. It’s important to note that back in the 1950s, these nodules were extensively studied, but that knowledge was lost for many years. We are now in the process of recovering that knowledge. The reasons for this oversight could be attributed to a “scientific eclipse” that occurred around the mid-20th century. The video explores the theory of the scientific eclipse in an amusing way. It is in Spanish, but English subtitles are provided.
PART 2: Useful information for HEALTHCARE PROFESSIONALS
Main questions about back mice…
- Part 2.1 – What are back mice, in simple terms?
- Part 2.2 – Are back mice considered lipomas?
- Part 2.3 – How can I suspect the presence of back mice?
- Part 2.4 – Why are these fibrofatty nodules called back mice?
- Part 2.5 – What are the main articles published regarding the topic of back mice?
- Part 2.6 – Why can back mice cause low back pain or referred pain?
- Part 2.7 – Why are many physicians unaware of the existence of this clinical entity?
- Part 2.8 – How can back mice be diagnosed?
- Part 2.9 – What are the treatment options for painful back mice?
- Part 2.10 – The best palpation technique
- Part 2.11 – How to perform an ultrasound examination
- Part 2.12 – How to infiltrate a painful back mice
- Part 2.13 – How to perform dry needling on a painful back mice
I recommend watching a 17-minute video presentation conducted in December 2022 in Poland. This video provides a comprehensive overview of our current understanding of the “back mice” phenomenon, including the main theories regarding the physiological underlying mechanisms. It serves as an excellent summary of what we know thus far about back mice. To access the video, simply click on the provided link.
Part 2.1 -What are back mice, in simple terms? (Information for HEALTHCARE PROFESSIONALS)
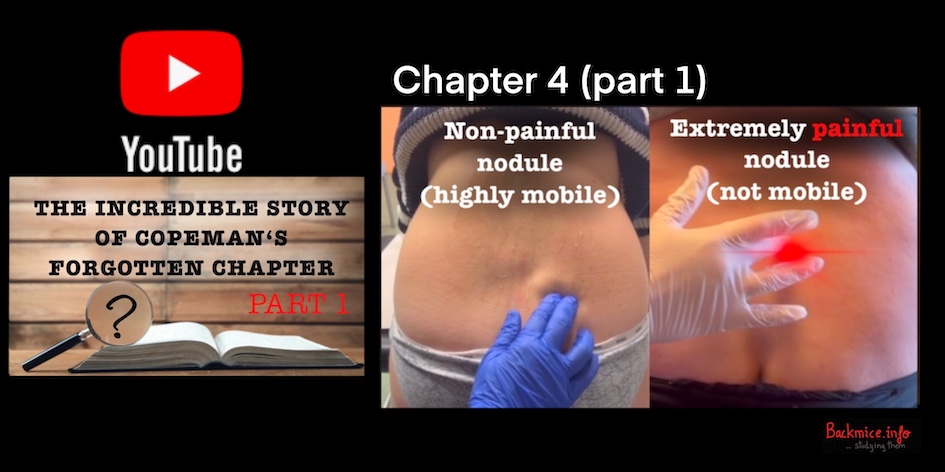
Simply put, back mice are deep palpable nodules composed of fibrofatty tissue located within the sacroiliac area. This area is a specific triangular region defined by the sacrum, iliac crest, and midline. These nodules are situated deep between the layers of superficial and deep fascia. Back mice can vary in size and number, as well as in terms of pain sensation. They can range from being painless to tender or even causing extreme pain upon palpation. Medical literature suggests that they originate from subfascial fat herniation, where deep fat protrudes to the surface. Despite their potential significance as a cause of low back pain, back mice are often disregarded or overlooked. However, the exact physiological pain mechanisms and herniation mechanism are still under investigation.
Part 2.2- Are back mice considered lipomas?(Information for HEALTHCARE PROFESSIONALS)
No, back mice are not lipomas. These nodules are formed due to a phenomenon known as “subfascial fat herniation.” Although there is a possibility of confusion between fibrofatty nodules and lipomas, especially if a doctor is unfamiliar with this topic, it is important to note that they are distinct entities. In the past, some doctors mistakenly referred to them as episacroiliac lipomas, but this term was a misnomer. It is crucial to recognize that back mice are not true lipomas; they are characterized by subfascial fat herniation.
Part 2.3- How can I suspect the presence of a back mice?(Information for HEALTHCARE PROFESSIONALS)
We can identify the presence of back mice through proper examination skills. Proper examination skills involve employing a correct palpatory technique, particularly using the fingertips along with the application of a suitable lubricant gel. If a healthcare professional is not familiar with these skills, there is a higher likelihood that they may overlook the presence of these nodules. The initial suspicion of back mice can be made through palpation, but the definitive confirmation of back mice should be obtained through an ultrasound examination.
Patients can consult with healthcare providers regarding two main clinical presentations related to back mice. The first presentation involves completely asymptomatic nodules that the patient discovers and becomes concerned about. The second presentation includes patients experiencing low back pain, whether they are aware or unaware of the presence of the painful nodules. Furthermore, by clicking the link, you can access a table summarizing the key clinical features associated with painful lumbar nodules (back mice) →LINK Table: Main clinical features related to painful lumbar nodules.
Part 2.4- Why are these fibrofatty nodules called back mice? (Information for HEALTHCARE PROFESSIONALS)
Throughout history, these nodules have been assigned various names. However, in the 1990s, Peter Curtis coined the term back mice for them. We have opted to use the term back mice consistently on our webpage, partly because it carries a somewhat amusing quality. Additionally, it is easier to pronounce compared to “subfascial fat herniations.”
For a comprehensive understanding of the different names attributed to these nodules, we recommend reading our published review from September 2021 titled “Historical Review of Studies on Sacroiliac Fatty Nodules (Recently Termed ‘Back Mice’) as a Potential Cause of Low Back Pain.” In this review, there is a table summarizing (→LINK Table: A brief history of some of the names of the lumbar nodules) the various names previously used to describe these fibrofatty nodules.
Part 2.5- What are the main articles published regarding the topic of back mice? (Information for HEALTHCARE PROFESSIONALS)
Even though back mice are often overlooked by mainstream medicine, there is a significant amount of medical literature dedicated to studying this clinical entity. Numerous physicians and healthcare professionals have published articles on back mice throughout history. Here is a link to access all the articles we have found.
→LINK to all of the published medical articles about back mice that we have found
The reasons why they continue to be overlooked in modern times despite having been studied are discussed below.
Our team’s initial step was to gather all the pertinent medical literature for further examination. In September 2021, our team published a comprehensive historical review that encompasses significant medical articles related to these intriguing lumbar fibrofatty nodules throughout history.
→LINK to a free on line PDF in the Pain and Therapy Journal → Historical Review of Studies on Sacroiliac Fatty Nodules (Recently Termed “Back Mice“) as a Potential Cause of Low Back Pain. Cañis Parera et al. Pain ther (2021).
Part 2.6 -Why back mice can cause low back pain or referred pain? (Information for HEALTHCARE PROFESSIONALS)
Although in most people these nodules are often painless upon palpation, leaving most people unaware of their existence. In certain individuals, the nodules are painful upon palpation, and patients may attribute their low back pain to these painful nodules or not. In such cases, proper treatment of the painful nodules can alleviate the low back pain, often with complete relief. This observation has prompted numerous medical professionals, including our team, to investigate these nodules and gain a better understanding of their nature and why they can sometimes cause low back pain.
Back mice have the potential to induce pain by compressing or irritating the superior cluneal nerves, which provide sensation to the skin of the lower back. When these peripheral nerves become entrapped, they can significantly contribute to the development of low back pain. However, the lack of recognition and understanding of back mice extends to the overlooking and awareness of the causes of superior cluneal nerve entrapment among healthcare professionals. These two entities are interconnected and often overlooked in clinical practice. For further information, you can access a list of published medical articles on the topic of superior cluneal nerve entrapment as a potential cause of low back pain through the provided →LINK to Chapter 2 – Nerve entrapment.
→LINK to This is a 27-minute-long video that aims to explain, in a very simple manner, how superior cluneal neuralgia can present as low back pain that refers to the leg. It is part of a translational project to transmit complicated knowledge in a YouTuber’s funny style. Anybody can understand the concepts explained there about neuropathic pain and all the associated symptoms. ENGLISH SUBTITLES.
The comprehensive explanation of the underlying pathophysiological mechanism behind the transition of nodules from complete asymptomatic status to extreme pain, even within the same individual, is elaborated in detail in Part 3 for researchers of the website, specifically focusing on the pathophysiological theories underlying the phenomena of back mice.
Part 2.7 – Why are many physicians unaware of the existence of this clinical entity? (Information for HEALTHCARE PROFESSIONALS)
Unfortunately, several factors have contributed to the neglect and underdiagnosis of this condition within mainstream medicine. These factors can be attributed to:
- Limited emphasis on palpation skills: Many physicians do not prioritize palpation during physical examinations, and as a result, they may lack the necessary skills to detect these nodules. Even when palpation is performed, the presence of the nodules can be easily overlooked without proper lubrication of the fingers or the patient being in the correct position.
- Confusion with conventional lipomas:There is a common misconception among some physicians that these nodules are similar to “conventional lipomas,” which are typically not associated with pain. This misperception can lead to the nodules being overlooked or disregarded as potential sources of pain. It is crucial to address this false dogma that fatty tissue cannot cause pain. In reality, fatty tissue dysfunction can be a significant pain generator that should be carefully considered rather than dismissed.
- Mistaken identity as myofascial trigger points: The nodules may also be mistaken for myofascial trigger points, further contributing to their underdiagnosis.
- Lack of visibility in imaging: These nodules are not visible on conventional radiography or basic magnetic resonance imaging (MRI), making them harder to detect through these diagnostic methods.
- Neglect of fibro-fatty tissue and fascia: The potential role of fibro-fatty tissue and fascia as causative factors in musculoskeletal pain disorders has been historically overlooked, further contributing to the underdiagnosis of these nodules.
- The lack of knowledge of histology and anatomy of these tissues: The lack of knowledge regarding these tissues stems from the general unfamiliarity among the medical community with the histology and anatomy of the fascia and fatty tissue.
- Lack of familiarity with cluneal nerve entrapment: Many physicians are not familiar with the existence and significance of cluneal nerve entrapment, which is associated with these nodules.
The nodules were extensively studied by a group of physicians in the 1940s and 1950s, and their findings were documented in reference books of that time. However, over the years, this knowledge seemed to have disappeared. After conducting a thorough investigation, we have developed our own theory regarding what could have happened. We address this subject in →Chapter 4 of our YouTube Channel “Diario de una investigadora”: “Los nodulos de copeman… historia de un eclipse científico” (Copeman’s nodules… the story of a scientific eclipse).
Part 2.8 – How can back mice be diagnosed? (Information for HEALTHCARE PROFESSIONALS)
…Under construction
Part 2.9 – What are the treatment options for painful back mice? (Information for HEALTHCARE PROFESSIONALS)
The treatment of back mice can vary depending on the individual, the severity of symptoms, and the recurrence of symptoms in the long term.
Conservative management: This approach may involve measures such as rest, activity modification, physical therapy, and the use of nonsteroidal anti-inflammatory drugs (NSAIDs) to alleviate pain and discomfort.
Localized interventions:
- Local anesthetic injections can be administered, and they may need to be repeated multiple times. LINK to the YouTube video Simple back mouse treated with local subcutaneous anesthetic injection.
- Multiply subcutaneous dry needling technique (with a 30G needle of 0.3mm x 8mm long) can provide pain relief and can also be repeated.
Surgical options: Surgical intervention should be considered when conservative measures fail to provide long-term relief, and the pain, despite improvements with infiltrations or dry needling, continues to recur, significantly impacting the patient’s quality of life. It is crucial to ensure that surgical removal is performed by a skilled surgeon who has experience with subfascial fat herniation and cluneal nerve entrapment.
VIDEO that shows how to performed a anesthetic block of a back mouse:
→ LINK to the video: Simple back mouse treated with local subcutaneous anesthetic injection.
Part 2.10 – The best palpation technique of back mice (Information for HEALTHCARE PROFESSIONALS)
In this appendix, we provide an explanation of the optimal palpation technique we have developed to help other healthcare professionals improve their ability to palpate these deep nodules. It is important to note that the lack of awareness of these crucial points has led to the current situation where many physicians are unable to detect these nodules. Therefore, the key points to remember are the patient’s standing position, the slight bend in their back (semiflexion), and the use of a lubricant during palpation.
- The recommended position for the patient is standing with a slight bend in the back (semiflexion) and hands resting on the examination table.
- Keep the area uncovered and apply a substance to your hands to allow for smooth finger movements. For instance, we use a sterilizer in these cases.
- Begin palpating the midline by applying firm pressure on the spinal apophyses. Ask the patient if they feel any localized pain.
- If the patient experiences pain on one side of the lower back, start with the painless side. Use your fingertips to palpate, using continuous circular movements to locate nodular spots.
- When the patient identifies a painful area, perform a second palpation and ask them to point out the spot of maximum pain.
- Apply firm pressure on the spot of maximum pain and inquire if the pain radiates to other areas such as the abdomen, inguinal region, gluteal region, or leg.
- Sometimes the nodules are only present on one side, while other times they may be bilateral. Sometimes there is a single nodule, while other times there are two nodules, with one above the other or even a cluster of nodules.
- Some nodules are tender or painful, while others are painless. It’s important to note that this can change over time, and a painless nodule can become painful.
- If we mark the nodules, they usually remain around 5-7 cm from the midline.The next video,
Chapter 3 of “Diario de una investigadora sin Glamour,” is a humorous explanation of the best techniques for palpating and locating back mice, as well as common errors that may occur without the proper skills. The video includes English subtitles to ensure accessibility for a wider audience.
 →LINK Capítulo 3: Solo palpar! (descubriendo el fenómeno “back mice”).
→LINK Capítulo 3: Solo palpar! (descubriendo el fenómeno “back mice”).
Part 2.11 – How to perform a ultrasound examination of back mice?(Information for HEALTHCARE PROFESSIONALS)
Any health professional who has a basic understanding of how to use an ultrasound can feel confident in performing an ultrasound examination of back mice. It is crucial to understand that the findings will differ between a non-painful nodule at the time of examination and a nodule that is sensitive or highly painful. Below, we will present the basic technique for ultrasound examination of a non-painful nodule.
Above in part 2.13, you will find a video presenting the ultrasound findings before and after the application of dry needling to a patient experiencing painful back mice. This video illustrates the changes observed in the ultrasound images as a result of the dry needling intervention.
Part 2.12 – How to infiltrate a painful back mice? (Information for HEALTHCARE PROFESSIONALS)
In the following video, you can see how to palpate and how to infiltrate simple lumbar “back mice” of a young patient who had right lumbar pain and referred pain to the posterior thigh since last 24 hours. The pain got worse with efforts or bending over.
She had past history of right lumbar pain some months ago, and some times she has lumbar pain randomly. When pressing the nodule the patient feels referred pain down the leg all the way to the knee. The pain disappears immediately after injecting 4ml 1% lidocaine. Pain relief lasted weeks.
Part 2.13 – How to perform dry needling on a painful back mice ? (Information for HEALTHCARE PROFESSIONALS)
… Under construction: Stay tuned for an upcoming video where we will demonstrate the dry needling technique that we employ
In the link provided below, you can watch a video that visually demonstrates the difference in ultrasound images of a back mouse before and after performing subcutaneous dry needling on a patient. The patient sought consultation for a six-year history of low back pain characterized by constant dull pain that worsened intermittently and in specific body positions. Palpation of the back mouse exacerbated the pain.
After performing multiple subcutaneous dry needling using a 30G needle measuring 0.3x8mm, the patient experienced pain relief, and the subsequent ultrasound examination revealed changes in the findings. These observations strongly suggest that puncturing the fascial layers produces objective changes that can be assessed through ultrasound imaging. These changes strongly support Copeman’s theory that the pain associated with back mice is caused by the presence of trapped lymph within the fascial membranes, leading to tissue tension. The ultrasound examination provides tangible evidence of the effects of dry needling as an intervention to treat painful back mice. The imaging helps visualize the improvements in the affected area, further supporting the effectiveness of dry needling in alleviating pain and addressing the underlying issue.
Please click on the link to view the video, which provides a graphical representation of these significant findings.
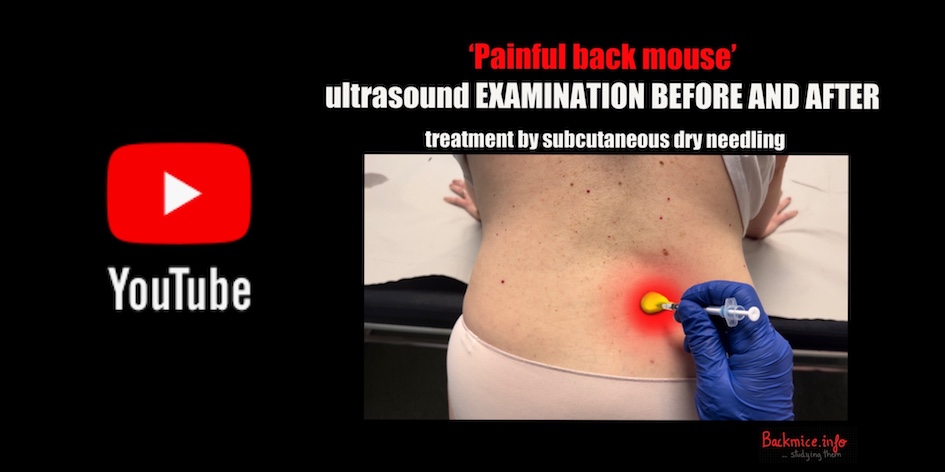 →LINK to a YouTube video where we show the ULTRASOUND IMAGES before and AFTER dry needling of a PAINFUL RIGHT SIDE BACK MOUSE (VIDEO with ENGLISH SUBTITLES)
→LINK to a YouTube video where we show the ULTRASOUND IMAGES before and AFTER dry needling of a PAINFUL RIGHT SIDE BACK MOUSE (VIDEO with ENGLISH SUBTITLES)
PART 3: Useful information for RESEARCHERS also studying this topic
Part 3 structure…
- Part 3.1 – Our theory regarding of “The scientific eclipse to back mice”.
- Part 3.2 – The intriguing stories of researchers who stumbled upon this topic by chance.
- Part 3.3 – A compilation of medical articles pertaining to this topic.
- Part 3.4 – The confusion surrounding medical terminology associated with this topic.
- Part 3.5 – Exploration of other clinical entities linked to back mice research.
- Part 3.6 – Remaining unanswered questions in the field.
- Part 3.7 – Our theories on lymphatic bubbles entrapped within fascial membranes.
Part 3.1 – Our theory of “the scientific eclipse to back mice” (specific content for researchers)
It is truly astonishing that such a significant clinical entity, back mice, has been largely disregarded by the medical community in the last 50 years. The perplexing reasons behind this oversight are explored further in this section. This remarkable historical account, once widely known, has the potential to revolutionize the way knowledge is transmitted in the future, to avoid repeating the same mistakes again.
YouTube videos Chapter 4: Copeman’s nodules (back mice)… the story of a scientific eclipse?
The YouTube series in Chapter 4 of my channel, “Diario de una investigadora sin Glamour,” is dedicated to exploring and presenting my hypothesis on a scientific eclipse. This series of videos aims to visually explain the events and circumstances surrounding this phenomenon. Although the videos are in Spanish, they are equipped with accurate English subtitles, making them accessible to a broader audience. Through these visuals, viewers can gain a better understanding of the topic and engage with the research I am conducting.
“The incredible story of ‘Copeman’s forgotten chapter’ is revealed in the following videos, showcasing how Dr. Copeman and his colleagues extensively investigated fatty hernias (back mice) and their potential correlation with back pain during the mid-20th century. Despite their groundbreaking discoveries and initial surge of interest, all this valuable knowledge was inexplicably lost and overlooked, leading to what may be recognized as one of the most remarkable scientific eclipses in history. This oversight likely resulted in unnecessary suffering for countless individuals.”
This chapter will be divided into several parts, each lasting around 5 minutes. Currently, parts 1 and 2 of the chapter have been published.
→ LINK to the video: Capitol 4 (part 1)
→ LINK to the video: Capítulo 4 (part 2)
Part 3.2 – The intriguing stories of physicians who stumbled upon this topic by chance (Specific content for researchers)
Despite the lack of awareness among most physicians today, back mice have been studied by numerous physicians from around the world throughout history.
Coincidentally, some of these researchers encountered this clinical condition by chance and were intrigued by it, just like us…
→LINK to the story of how we became fascinated by back mice, ‘my personal story’. →LINK to the story of how Dr. H. Austin, one of our collaborators, performed his first surgery on a patient.
Similar stories to ours have been documented by several physicians in published articles. We recommend exploring the cases of →Dr Ries, Dr →MacDermont, →Dr Clavero-Núñez (in Spanish), and →Dr Monnerot-Dumaine, among others.
Part 3.3 – A compilation of medical articles pertaining to this topic (Specific content for researchers)
If you are interested in researching back mice, you may find our list of published medical articles on the topic valuable. The articles are listed in chronological order, providing a historical perspective on the subject. Additionally, if you are interested in accessing the original PDF versions of the articles, please feel free to contact us (contact@backmice.info), and we will gladly provide them to you free of charge.
→LINK to ALL the published medical articles about back mice
However, for a better understanding, we highly recommend referring to our review published in 2021. This review serves as an excellent summary of all the research conducted on back mice thus far. It offers a comprehensive overview of the topic.
Back mice have been found to be potentially related to cluneal neuropathy. In the link provided below, you can access a comprehensive list of articles that have studied this peripheral neuropathy.
→LINK to ALL the published medical articles about cluneal neuropathy
Part 3.4 – The confusion surrounding medical terminology associated with this topic (specific content for researchers)
Back mice is one of the many names that the LUMBAR FIBRO-FATTY NODULES have received (Back mice was a name proposed by Peter Curtis on the 90’s).
Many doctors have been intrigued by the study of these mysterious and painful nodules, and it appears that each one has chosen a different name for them. Above, you will find a list of these names, each linked to a summary of the corresponding medical article we could find. The nomenclature surrounding these nodules is in a state of chaos and confusion.
We have gathered articles ranging from 1843 to the most recent ones. One thing is certain: physicians in the past were more familiar with palpation skills, and the presence of deep fibrofatty nodules or indurations was a significant and important issue they endeavored to investigate thoroughly.
We have presented the list as such because it visually represents the chaos. You can access a table in this link (→LINK to the Table: A brief history of some of the names of the lumbar nodules) , which summarizes the main names that back mice have been given throughout history.
List of names and studies about these nodules during history:
- Rheumatic effusion or induration -Hautschwiele, Zellegewebesschwiele, Muskelschwiele or Knochenhautschwielen- (Froriep 1843)
- Swollen fibrous indurations (→Stockman 1904)
- Cellulalgic nodules or cellulite nodule (→LINK to french studies)
- Subcutaneous fatty nodes (→Sutro 1935)
- Epi-sacro-iliac lipoma (→Ries 1937)
- Sacroiliac nodules (→MacDermot 1942)
- Fibrositis of the back (→Copeman and Ackerman 1944) (→Mylechreest 1945), (→ other articles about fibrositis)
- Fibrositic nodules (→Pugh 1945)
- Herniation of subfascial fat (→Herz 1946) , (→Hench 1946), (→Hucherson and Gandy 1948) (→Herz 1952) (→Bonner 1954)
- Painful lipomas (→Rouhier 1951)
- Herniation or oedema of fat lobules (→Copeman and Ackerman 1947) , (→Copeman 1949) (→Clavero-Núñez 1945)
- Nodulation or herniation of fat (→ Moes 1947)
- Fibrolipomatous nodules (→Orr et al. 1948)
- Episacroiliac lipoma (→Hittner 1949), (→Katz 1950), (→ Sicard 1952), (→1952 Donati and Bidoni) (→Sheehan 1953), (→Monnerot 1955), (→Nocentini and Rosati 1956) (→Pace and Henning 1972) (→Rosati 1990), (→Beverley 2007).
- Hernia grasa (→1946 “El día médico”) (→1950 Dal Lago &Vera)(→1953 Nunziata)
- Pannicular hernia (→Ficarra 1952) (→Knight 1954) (→Ficarra 1955) (→Tong 1981)
- Sacroiliac lipomatosis (→Raymond 1952), (→Raymond 1960)
- Lipomatose kreuzbeinsyndrom (→Schmidt-Voigt 1953)
- Hernia of the panniculus adiposus (→Gomez 1957)
- Hernia of the sacral fascia (→Kanan 1959)(→Tibaudin 1959)
- Sacroiliac (episacral) lipoma (→Wollgast and Afeman 1961) (→1990 Grieve)
- Lipomes épi-sacro-iliaques (→Rimbaud 1953), (→Duval 1962)
- Hernia adiposa (→Sedwitz and Thomas 1963)
- Lipomata in sacroiliac region (→Singewald 1966)
- Copeman and Ackerman syndrome (→Baciu 1969)
- Lumbar fat herniation (→Faille 1978)
- Xanthoadipose nodules (→Ercegovac 1982)
- Non-fibrositic lumbar subcutaneous nodules (→Swezey 1991)
- Back mouse/mice (→Curtis 1993) (→ Fischer 1993), (→Earl 1995) (→Motyka 2000), (→Curtis 2000), (→Bond 2004), (→Curtis 2004), (→Bicket 2016), (→Tiegs-Heiden 2017) (Cañis-Parera et al. 2021)
- Iliac nodular disorder (→Kurnik 2003)
- Episacral lipoma (→Bond 2000), (→Erdem 2013)
- Fibro-fatty nodule (→Su Min Ko 2009)
- Sacroiliac fascial Lipocele (→Yang 2015)
- Nodolo di Copeman (→Farina 2017)(→Martinze-Nuñez 2020)
Other names for specific sacroiliac pain:
- Multifundus triangle syndrome (→Buwens 1955)
- Lumbodorsal subfascial fat fibrosis (→Dittrich 1963)
- Iliac crest pain syndrome (→Collée et al. 1991)
→LINK to ALL the published medical articles about back mice
Part 3.5 – Exploration of other clinical entities linked to back mice research (Specific content for researchers)
Surprisingly, we discovered that many clinical entities are somehow related to back mice.
- The relation with fibromyalgia: However, before the term “back mice” gained popularity, these nodules were described as a clinical presentation of a condition called “fibrositis.” Specifically, they were referred to as “nodules due to lumbar fibrositis,” particularly in England. Over time, the term fibrositis fell out of use as it was considered a misnomer. Patients who presented with multiple nodules throughout their bodies, including the lumbar area, were said to have “primary fibrositis.” Eventually, this term transformed into the current term “fibromyalgia.” It is worth noting that many patients diagnosed with fibromyalgia commonly exhibit bilateral back mice. However, further study is needed to better comprehend this correlation.
→LINK to The history of the term “fibrositis“ (an old name for back mice was lumbar fibrositis and an old name for fibromyalgia was generalized fibrositis)
- The origin of the French term “cellulite”: In the past, the deep fatty tissue was referred to as “cellular tissue.” The term “cellular tissue” was used as a substitute for loose connective tissue ( currently, there is a trend to refer to it as “deep fascia”). However, in France, the pain originating from this deep fibro-fatty tissue was termed “cellulite” (using the term to describe pain in the cellular tissue) or “cellulalgia.” Surprisingly, the term “cellulite” for pain has disappeared and is now primarily used to address the visual aspect of fatty tissue, mainly related to aesthetic concerns. However, at the beginning of the century, it denoted pain, and the nodules in the lumbar region were referred to as “lumbar cellulite.”
→LINK to the French studies about the “cellulite“ (an old name for back mice by French doctors was lumbar cellulite)
- Myofascial syndromes: Myofascial syndromes refer to a group of conditions characterized by the presence of myofascial trigger points. These trigger points are hypersensitive points that can cause local or referred pain, muscle stiffness, and restricted range of motion. There can be confusion between myofascial syndromes and the tender nodules found in back mice, as they share similarities. It is possible that these two conditions are related in some way, further emphasizing the need for research and exploration into their connection.
→LINK to the articles about the myofascial syndrome (another view for back mice)
- Other clinical entities related to back mice include the German terms “myogelosis” and “muskelhärte,” which refer to similar conditions characterized by localized muscle tightness and tension. It is important to note that back mice can be mistakenly confused with these entities. Therefore, ultrasound imaging plays a crucial role in confirming whether the palpable nodules or indurations are indeed located within the fascial layers rather than the muscle fibers.
→LINK to the articles about myogelosis [myogelose and muskelhärte] (another view for back mice)
Part 3.6 – Remaining unanswered questions in the field (Specific content for researchers)
Below, you will find a list of questions that we had when we started our research in 2017. To be honest, many of these questions still require further research to provide comprehensive answers.
- What are back mice, the fibro-fatty lumbar nodules, exactly?
- How are they related to low back pain and other pain syndromes?
- Why do they sometimes exhibit tenderness or pain while other times they remain asymptomatic?
- Why have the studies conducted by W.S.C. Copeman and others been overlooked?
- Why are they identified as nodules by some and as trigger points by others?
- Why do the tender nodules sometimes manifest as lobules under tension and other times as herniations?
- Why are they predominantly bilateral?
- Why do they form a bubble of fat?
- Can they become painful due to edema, hemorrhage, congestion, or torsion?
- Does the edema respond to hormonal or sympathetic stimulation?
- Why can recurrent painful edema occur?
- Are they composed of brown adipose tissue?
- Why can they sometimes be alleviated with anesthetic injection alone or dry needling?
- Why is surgical removal necessary in certain cases?
- During surgical incision, why do the tender nodules protrude due to edema and tension?
- What causes subfascial fat herniation?
- What are the subfascial basic fat pads?
- Can these nodules cause cluneal nerve entrapment?
- Why are they associated with fever or humid coldness?
- Why is fatty tissue so poorly understood?
- Why do many physicians lack the skills to palpate them?
- Why do they have numerous names?
By 2023, we have managed to partially answer some of these questions, but there is still much work to be done. These questions emphasize the necessity for further research and exploration to gain a deeper understanding of back mice and fibro-fatty lumbar nodules.
Part 3.7 – Our theories on lymphatic bubbles entrapped within fascial membranes.
The pathophysiological theories underlying the phenomena of back mice (the theories behind the pain mechanisms):
The most perplexing puzzle surrounding back mice is the enigma of how nodules can transition from a state of complete asymptomatic status to extreme pain, even within the same individual over the course of their lifetime. This conundrum, as highlighted by Dr. Hench in his article, has challenged researchers to comprehend the underlying pathophysiological mechanism responsible for such fluctuations.
According to Copeman and other researchers, the fluctuation in pain intensity is correlated with the amount of water trapped within the fascial membranes. If the lymph can be reabsorbed within a few days, the pain tends to dissipate on its own. However, if a significant amount of water becomes trapped, the pain can become chronic, even for years.
Additionally, the degree of tissue tension resulting from this trapped edema may explain the varying levels of pain experienced, including the potential involvement of superior cluneal nerve entrapment. Some researchers have even observed fatty esteatonecrosis within surgically removed nodules, indicating the presence of high tissue tension.
Furthermore, surgeons who have removed herniated fat have reported that upon opening the initial layers, the herniated fat “pops up,” providing evidence of tissue tension.
The theory is indeed supported by the observations made by many researchers who have found that needling the nodules significantly improves the associated pain, whether or not local anesthesia is used during the procedure. Copeman described this technique as the teasing needling technique. It is noteworthy that various pain therapies employed today utilize needle-based interventions for localized pain relief, such as anesthetic infiltrations, dry needling in physiotherapy, acupuncture in traditional Oriental medicine, prolotherapy, mesotherapy, neural therapy, and more.
These therapeutic approaches underscore the potential effectiveness of needle-based interventions in addressing localized pain, further bolstering the concept that needling the back mice nodules may provide pain relief by disrupting the fascial membranes with trapped lymph. Our recent ultrasound findings conducted before and after dry needling lend support to this theory, indicating that it may indeed be valid.
These intricate observations shed light on the multifaceted nature of back mice and the underlying mechanisms that contribute to the spectrum of pain experienced by individuals. Exploring these complexities is vital in unraveling the mysteries surrounding back mice and advancing our understanding of this intriguing phenomenon.
Thank you for visiting our website!