Mylechreest dissected 12 bodies 1945 and concluded that fatty tissues may play an important part in the pathology of the fibrositis of the back (also known as back mice).
Notes on the article of:
Investigation into the Aetiology and Pathology of Fibrositis of the Back
Mylechreest WH.
Annals of the Rheumatic Diseases. 1945;4 (4):77-79.
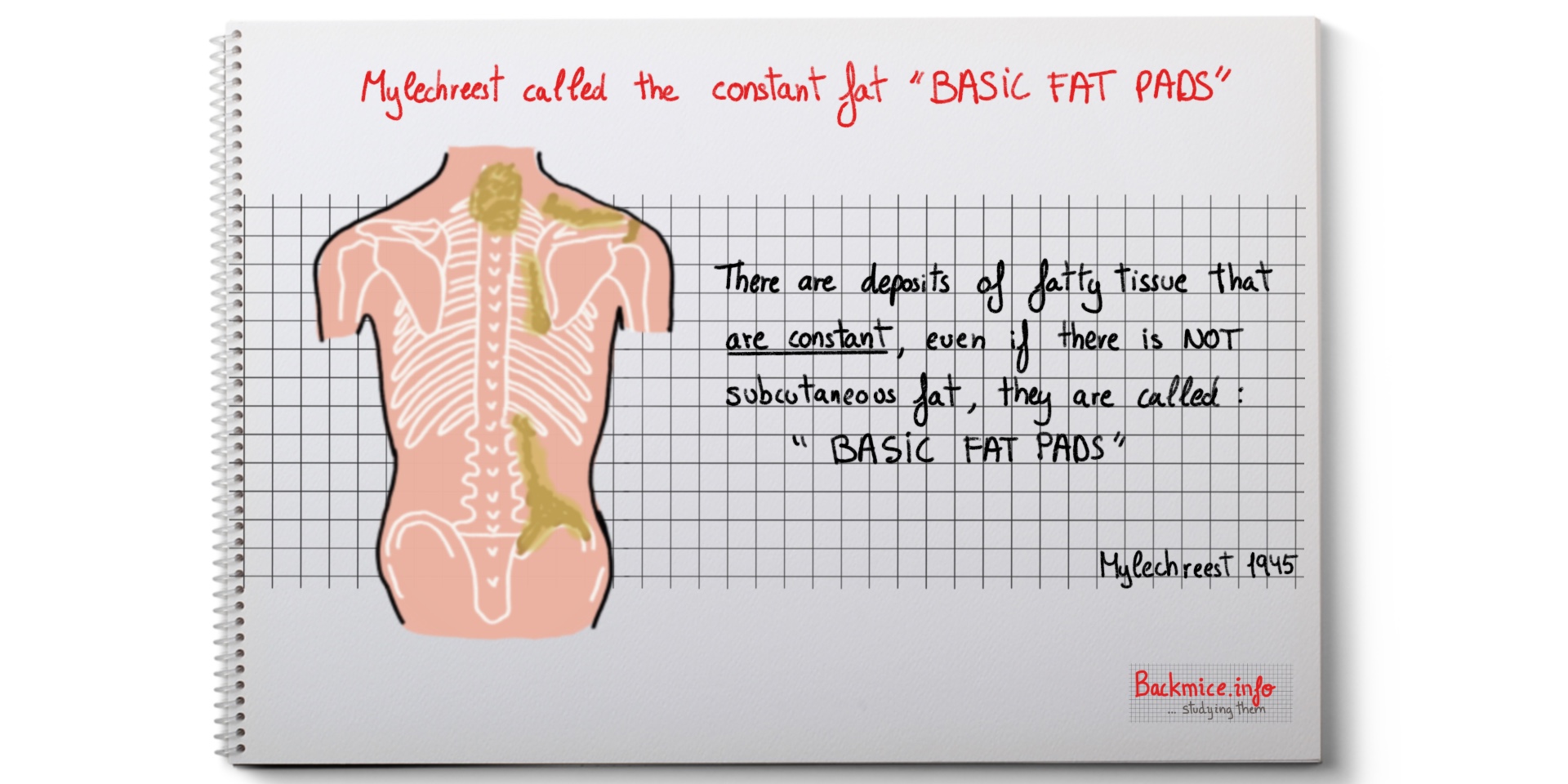
Mylechreest starts saying that the aetiology and pathology of fibrositis of the back are still unknown. With this investigation he hopes “to clarify the picture”. He states that the constant occurrence of the basic-fat pattern in all the backs dissected, even in those which had no subcutaneous fat suggests that the fatty tissues may play an important part in the pathology of the “fibrositis” of the back.
First he dissected 12 bodies to study the fatty tissue
He decided to examine the backs of all bodies reaching the post-mortem table to establish the “normal” condition before studying the “fibrositic” nodules. He dissected 12 backs from the first twelve bodies that came. This included bodies from long-standing illness and bodies of sudden death.
As the “findings” were constant they were regarded as “normal”. The important role that fatty tissue might play in the disease became apparent after examination of a few backs. He also got the opportunity to see the biopsy material from Copeman and Ackerman (1944), which provided him additional evidence.
The striking feature of the “basic fat”
-The most striking feature of these dissections was the distribution of fatty tissue apart from the subcutaneous fat.
-This fat was constant in all the bodies, even if they had little or no subcutaneous fat; therefore, they called it the “basic fat”.
-The superficial fascia extends over the entire surface of the body and contains a VARIABLE AMOUNT of fatty tissue.
“The basic fat” in the back
-Superficial fascia consists of many layers and compartments. In this article, the term superficial fascia is restricted to this second or deeper superficial fascia. Deeper into this, there is the deep lumbar fascia.
-Deep lumbar fascia consists of 3 layers: posterior, middle, and anterior. Posterior and middle layers: unite at the edge of M. Sacroespinalis (M. Erector spinae) to form the sheath for the muscle. The fat enclosed in this angle thus formed plays an important part in “fibrositis of the back”.
ZONE 1 (from the neck down to the lower costal margin)
Superficial fascia in the region of the shoulder
-It gets thicker as it ascends to the top of M. Deltoids; there are deposits of yellow fat in the upper and posterior aspects of the joint.
-The fat tends to run into the intermuscular septa.
-It thickens into a stout band superficial to the posterior aspect of acromion and superior border of scapula.
-The fascia is very adherent to skin except between the scapulae.
-A thick fibrous fascia (deep fascia) was found over M. Infraspinatus, with fibres just visible to the naked eye running downwards and outwards. It was attached and forms a capsule for the muscle.
-Some fat was found along spinae deep to this fascial attachment.
-At the angle by two layers of fascia that enclose the M. Trapezius there was some fatty tissue.
–Fat in zone 1 is entirely yellow in striking contrast to that in zone 2. It is mostly deep to the superficial fascia and found chiefly on the inner side of the scapula and the point of the shoulder.
-There is yellow and pink fat lying in the sheaths of the tendinous portions of the erector spinae muscles deep to the trapezius and rhomboids.
-There is an area of fat in the midline extending from the level of 5th cervical vertebra to the 3rd thoracic: this fat lies on and in the superficial fascia.
ZONE 2 (from the lower costal margin to the iliac crest)
– In this zone superficial fascia is very vascular, fine hairlike vessels can be seen clearly.
-The skin is more adherent in this zone (except towards the side).
-The most striking feature is that the “basic fat” is reddish.
-There are compartments:
- Medially: outer border of M. Sacroespinalis.
- Laterally: It reaches the iliac crest and is some 2 1/2 inches lateral to the outer border of M. Sacroespinalis.
- Above: The level of 3rd lumbar vertebra.
- Below: it descends for some 2 inches below iliac crest and covers a part of M. Gluteusmedius (which is not covered by M. Gluteus maximum).
-There is fat in the angle formed by the posterior and middle layers of deep lumbar fascia where they unite to enclose M. sacroespinalis. It extends up to the point where M. sacroespinalis is crossed by lower border of M. Latissimus dorsi. PRESUMABLY protecting the nerves and blood vessels, which perforate this fascia where they are not covered by the latter muscle.
-The red fat from zone 2 extends to this zone.
-The rest of the fat is yellow and is considerable in amount; it lies in and deep to the superficial fascia.
HERNIATION OF FAT and its relation to fibrositis
-He observed herniation of fat from one layer to the other.
-By pressure, he could bring one lobule by either side of a weak spot in fascia (he supposed then that the sudden contraction of muscle could provoke herniation by pressure).
-On 12 biopsies on selected patients who suffered “fibrositis“, he found fatty lobules under tension or fatty herniae. Their removal resulted in cure, or striking relief. He performed twelve biopsies in patients (a part of the twelve dissections).
-NERVE ENTRAPMENT: He described the fat pads in the angle formed by union of the posterior and middle layers of the deep lumbar fascia. The posterior primary nerve roots pierce this fascia there and are surrounded by fatty tissue. Congestion or oedema of this fat could obviously give rise to severe pain, furthermore, the edges of the ring of fascial opening might maintain these swollen lobules for a long time, resulting in permanent pathological change.
He divides the herniae into two groups
–Congenital: The mass of fat passes through one or more layers of fascia through well-defined gaps (found many times in the course of dissections).
–Acquired: mechanical or postural (i.e. lying in bed during long illness).
Other considerations about symptoms in case of fat herniae:
-The mere presence of herniation will not necessarily give rise to symptoms by itself.
-The herniation could take place by mechanical means (i.e. during violent physical exercise or unexpected contraction of certain muscles) which could lead to constriction of blood vessels, leading to oedema or haemorrhage in fatty tissue (this was confirmed by examination of biopsy and the history of the patients in 2 cases).
-Oedema is likely to arise in postural cases, and congestion may follow in febrile illness (one patient developed acute fibrositis during an attack of infective hepatitis; the biopsy showed a large non-pedunculated herniating fatty lobule under considerable tension).
-Many other fatty lobules taken had fibrous pedicles; the pedicle runs from one fatty lobule to another. Sections showed young fibrous tissue growing into adipose tissue. It may lead to the formation of a pedicle with years. It is easy to imagine torsion of that pedicle.
Therefore, the causes of pain could be:
- oedema (i.e. prolonged lying)
- haemorrhage (i.e. trauma or physical exertion)
- congestion (i.e. febrile illness)
- torsion of pedicle
Four case reports (of the many which were seen) related to fibrositis patients
CASE 1. Man with history of lumbago. Backache after physical exertion. On examination, he had very tender spot at the outer edge of M. Sacropinalis at the level of the third lumbar vertebra. Slight thickening could be felt but no nodule could be palpated. After incision was made to deeper layers, the protrusion of small herniation was exposed. The fat herniation was removed with a small area of fascia. After 14 days, patient was cured. Microscopic examination showed fatty tissue with young very cellular fibrous tissue growing into it. The blood vessels were congested and there was some haemorrhage into the tissue. There were also areas of older fibrous tissue. And serous exudate into some of the fat spaces.
CASE 2. Patient with history of intermittent backache. Pain for 15 years after an accident when playing football. The pain was lit up by damp weather, cold winds, and attacks of influenza. A tender spot over the crest of right ilium could be palpated, local pressure produced pain. After incision, a fat lobule was found lying superficial to the gluteal fascia. The lobule had a vascular pedicle going through the fascia to another lobule lying deeper. After removal, the patient was cured. The section of tissue consisted of fatty material invaded by young and very cellular fibrous tissue with patches of older fibrous tissue. The nodule was relatively avascular.
CASE 3. Patient with backache for 4 yrs. Pain first noticed after sleeping on damp ground. The pain radiated from the back till the buttock, back of the thigh, knee and calf. It tended to recur with chills. There was an easily palpable nodule at outer border of Erector Spinae, just above the iliac crest. Pressure reproduced the pain. On incision, fat nodule of the size of a cherry was found. It had a vascular pedicle, which ran through the superficial fascia. Removal cured the patient.
CASE 4. Patient with severe pain in buttock and back of thigh for a year. Not known cause. Pain worsened after lying in bed. Pain flared up during an attack of infective hepatitis. A tender nodule was found in the buttock 5 inches from midline and 2 1/2 inches below iliac crest. Injection of 10cc of 1% novocaine and teasing with thick needle gave much relief. But tender nodule was still present. Three layers of fat were found after incision with some lobules being under tension, building up into the bound when the septa were cut. One nodule the size of a pea was removed, the rest teased and broken up. Patient became free from pain after 18 days.
Published in March 2018By Marta Cañis Parera 
contact@backmice.info
References
- Mylechreest WH. Investigation into the Aetiology and Pathology of Fibrositis of the Back . Annals of the Rheumatic Diseases. 1945;4(4):77-79.
- Copeman WS. Aetiology of the Fibrositic Nodule. Br Med J. 1943 Aug 28;2(4312):263-4. PubMed PMID: 20785002; PubMed Central PMCID: PMC2284845.