(First, please check our video posted in October 2023 on "Cluneal nerve entrapment" and the "back mice phenomenon")
Back mice is a colloquial term that has been popularized to named the painful palpable fibro-fatty nodules of the sacroiliac area (The term was coined by Peter Curtis in 1993, In the search of back mouse).
An overlooked medical condition and the wrong dogma
Since back mice is a condition that is still overlooked by mainstream medical practitioners. The first diagnostic orientattion for these lumps is ‘lipoma’ and the dogma is that “Lipomas do not hurt”. But back mice are not lipomas. As the back mice go misdiagnosed, the worried patients look for the answers on the internet as the pain is still there.
The role of the social media
These days internet has become a shelter for patients to search for information and share their symptoms and experiences to help each other. Gladly, the patients of back mice can find the information on:
- Our web page www.backmice.info
- “Are Back mice real?” of www.verywellhealth.com
- “What in the world are Back mice” www.academyofclinicalmassage.com
- “The problem with the back mice” massagetherapy.com
- “Episacral lipomas” www.physio-pedia.com
Apart from the literature, youtube also has some videos providing information on the topic of back mice. The most watched video (with more than 254 thousands views) is “Lumps in Low Back, Top of Hip” where Chiropractor Hilma Volk has provided a comprehensive information in a very simple manner for general audience. Tnere are some some facebook pages where people are discusing their journey through the pain of back mice.
Are the plastic surgeons resolving low back pain?
After my research of reading through these social media forums for back mice, I found that lot of patients are posting stories of their journey through the pain and in some cases ultimately overcoming the pain through surgery performed by plastic surgeons.
So, after all the social media stories and the medical research available the question still remains open, “Is surgery the ultimate solution to this condition?” Well, until the mainstream medicine fully understands the cause of these painful fatty lumps and finds a less invasive way to cure these, I think we would have to resort to the plastic surgeons for the severe cases.
Published by Marta Cañis Parera in Novembre 2021
The scientific eclipse to back mice?
“The incredible story of ‘Copeman’s forgotten chapter’ is revealed in the following videos, detailing how Dr. Copeman and his colleagues investigated fatty hernias (back mice) and their potential relationship with back pain in the mid-20th century. Despite early discovery and a surge of interest, all this knowledge was lost and overlooked, in what is now considered one of the most spectacular scientific eclipses in history. This oversight may have resulted in unnecessary suffering for countless people.
“Copeman’s nodules (back mice)… the story of a scientific eclipse?
->LINK to Youtube: Chapter 4 (Part 2): What did they mean by Non-articular rheumatism. (5 minutes long) english subtitles
-LINK to Youtube: Chapter 4 (part 3)…. coming soon
Other links to Youtube Videos


1. If pressing on it does not hurt, is it still a back mouse? The whole area hurts for weeks after weightlifting.
2. Is there a non-surgical way to remove or minimize the bump (dry needling, injection, puncturing)?
3. Can it cause pain in the erector?
Dear Malcolm,
Thanks for your questions.
1. If pressing on it does not hurt, is it still a back mouse? Yes. “Back mouse” it is just a term to name the deep fibro-fatty lumps that can be felt in the sacroiliac area. Most of the times they are not painful while pressing on them. Whereas, sometimes, these nodules can be very painful in certain patients (that is what we are currently studying).
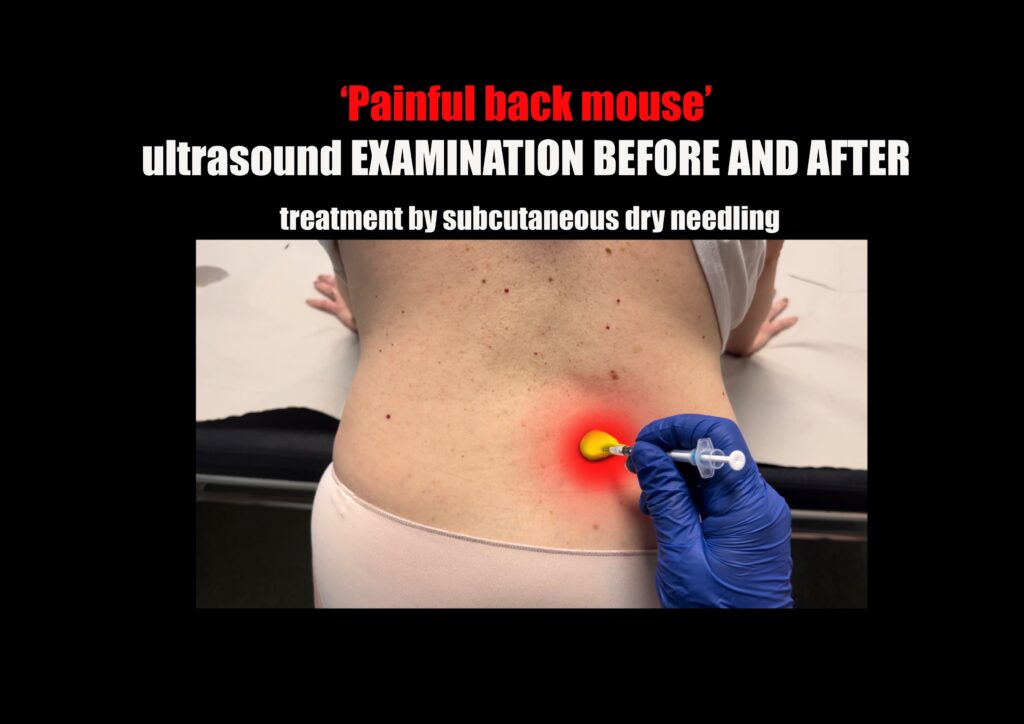
2. Is there a non-surgical way to remove or minimize the bump (dry needling, injection, puncturing)? Yes. Dry needling, anesthetic injection, and other types of puncturing the nodule have been report as being effective methods for pain relief in some patients.
3. Can it cause pain in the erector? Yes. It is said that can cause associated muscle spasm in the erector.
I hope I could help you.
Saludos
Marta
Marta,
Do the treatments you listed make the lump smaller/go away, or are they only for pain relief?
Hello Malcom,
As far as I know these treatments have been reported as being effective for managing the pain in a short or long basis, lumps usually persist, but pain goes away. In most people the lumps persist for long time, and pain seem to come and go.
Saludos,
Marta
Very interesting work Dr Marta. I suffer from this same back mice just above my left iliac crest. Being a general surgeon myself, I hoping to get a colleague to remove them under LA and send the specimen off to histopath. Is closing the fascial defect and absolute must to prevent a recurrence?
Dear Malcom,
Some surgeons mentioned that in some of the studies. Indeed, closing the fascial defect was recommended by many surgeons that had published about back mice.
Marta Cañis Parera
If we are only going as deep as the basic fat pad and the resulting deep fascia; I assume that having a general surgeon or cosmetic surgeon can perform this; with minimal to no risk to any nerves… correct?
God its a curse. I cant do my job any more. I’m in New Zealand, have seen physios, GPs & chiropractors. All of them say they wont operate & pass the buck. But its a matter of persisting until you find a surgeon that will do it.
I tried ultrasound fat cavitation to shrink them – only seemed to work minimally. DMSO, electro current etc – tried it all.
I met some old Chinese ladies & they said over there they just cut them out no problem.
mine dont hurt when I touch them at all. but its the nerves they touch against that hurt
Found an orthopedic surgeon that is a tumor specialist. Getting MRI next week. Ultrasound confirmed the Lipomas. Hopefully surgery will fix it.
Hey Gareth! Hope you’re currently ok regarding your back mice. Did you end up having the surgery? I’m considering the same. Please let me know if it worked for you. Thanks.
Hello. I just had a surgery for this , I had 2 one the left side and one on the right side, in the back, sacroiliac area. After 4weeks the one in the right is perfect, but the other one in the left side sincer 5days is hurting me a lot and also some pain in the buttock, I think due to cluneal nerves, because nothing bad with my spine. Any advice please about doctor that threated cluneal nerves? Or this. Thank you Adriandragos90@yahoo.com
Hello Adrian, I will send you an email to see if I can help you in any way
Marta Cañis Parera
Hello Adrian, did you ever get sciatica pain going to your leg on the side you had your lipoma removed? If so, when did you start noticing you no longer had sciatica after removal? I just had mines removed (episacral lipoma) which caused me very uncomfortable sciatica pain down my leg.
Greeings Marta,
After further research, it appears my lump begins at the Inferior Iliac Spine, instead of the oft mentioned Superior. Also, it is diagonal instead of transverse, and more linear than oval. Does this still sound like an episacral lipoma?
I saw a dermatologist today and mentioned the site. Although it felt soft to me, the doctor said it felt harder than it should and she was not sure it was a lipoma, and ordered an MRI, I guess to rule out other back pain sources. If it’s clear, the next step I’ll ask for is an ultrasound.
Dear Malcom,
The gluteal area around the iliac spine, is also a place were the back mice could be found. They could be called ‘gluteal mice’. But not EPISACRAL lipoma. Ultrasound is a better examination method for the time being for this fibro-fatty lumps.
Saludos,
Marta
Sorry Marta last question. Do you know if the people who had it successfully removed had it simply excised, or was there also a “defect” in the fascia that needed to be repaired. Of the two videos I saw on YouTube it was a simple excision. But how would a dermatologist/plastic surgeon know, and be qualified to fix a “hernia”? Are there two different variants of back mice, one that simply begins on top of the fascia, and one that punctured through it?
Dear Malcom,
According to the literature, the surgeons not always found a fascial defect. Sometimes the surgeons described a clear fascia defect in the thoracolumbar fascia that they repaired, but other times that was not found, nevertheless the pain was relief. So probably, as you mention, it may be “different variants of back mice”.
What seemed to me a common finding is that many surgeons described that the painful lumpy fibro-fatty tissue appeared edematous and under tension: “the lumps of fat popped out as soon as excision was performed as a sign of confined tension”. They commonly described that the edema was confined under a thin fibrous capsule.
A dermatologist/plastic surgeon could be perfectly qualified to fix that. Of course, we first need to better understand this overlooked condition. And specially the local irritated peripheric nerves that cause the pain, the superior cluneal nerves.
Saludos,
Marta
Marta, is it possible for it to not be in encapsulated at all? Just a nonuniform, jagged piece of fat with no shape whatsoever?
Hello,
According to the studies, sometimes the back mice can be felt just like an LOCALIZED INDURATION of the fibrous-fatty tissue. So, yes!.
Saludos,
Marta
I have the symptoms described and had an ultrasound done. The diagnosis was a lipoma. Met with a surgeon who said he could remove them but said it is unlikely to resolve my pain. Met again with my doctor who has suggested getting an MRI to rule out any other issues so I have that scheduled in 2 weeks. In the meantime I tried dry needling but not sure if the therapist actually dry needled into the lipoma/back mouse or around it. Didn’t seem to help much.
Should I just get the surgeon to remove it or should I search for a doctor who might be more familiar with this issue? I asked my doctor for a steroid shot into the area but he wasn’t comfortable doing it
Before surgical removal, a diagnostic test needs to be performed. Injecting 2-4 ml of local anesthetic into the painful nodule is enough to confirm that the pain arises from that area, due to the compromise of the terminal branches of the superior cluneal nerve network. Remember, surgery should be conducted by a surgeon who is knowledgeable about the back mice phenomenon and the superior cluneal nerves. Before considering surgery, several anesthetic blocks can be repeated; sometimes, this provides long-term relief. Dry needling to alleviate pain from a back mouse is demonstrated in the following video: https://youtu.be/DgNP4Ysl1hk?feature=shared
Hi Marta,
Just got my ultrasound:
“No discrete sonographic correlate for the indicated palpable abnormality.
Please note that an unencapsulated lipoma could potentially be sonographically occult.
At the indicated site of palpable abnormality, there is no discrete solid mass or focal fluid collection. No lymphadenopathy. No inflammatory changes in the imaged soft tissues.
Limited comparison imaging of a similar area on the contralateral side is also unremarkable.”
So it sounds like they saw nothing, but said if I had an unencapsulated lipoma, it may not show up anyway. I have an MRI scheduled now, which I understand has rarely shown the lipoma.
Have you had patients who had the condition but ultrasound showed nothing? I don’t know what to do at this point. Thanks so much.
Essentials of Orthopedic Surgery P168 says they dont usually show with ultrasound but at least it does acknowledge them
Hi Gareth,
Could you email me at contact@backmice.info and send me this info you mentioned?
Saludos,
Marta
Hello Malcolm,
Yes, it has been described that sometimes the painful fatty mass (back mice) is not really visible in the ultrasound (and it is mainly not visible in MRI).
But if the LOCAL ANESTHETIC INJECTION into the palpable fatty mass can give relief of the symptoms, then that is a clue for diagnosing LOCAL CLUNEAL NERVE IRRITATION (due to back mice).
The main reason that science is overlooking this condition is that it is really challenging to be understood and diagnosed. The FIBRO-FATTY tissue (fascia) and its abnormalities like ‘back mice’ have been neglected as a pain generators and nerve irritators because of its anatomical and phisiological complexity.
Unfortunately, there are many questions that remain to be answered.
Best whishes,
Marta
Dear Dr. Parera,
Question: Where can I find a physician to investigate my suspected “back mice” near me or somewhere is the Midwestern US?
History: I am a 43 y/o, 5’8″, 180lb, 7th yr registered nurse with an athletic build who has had lower back pain and referred hip/thigh/leg pain for years (even before nursing) and recently discovered the masses you describe after an occupational injury while applying a lidocaine based cream to the area. I suspect that they may have been there for a long time as symptoms are reproduceable with palpation of the “lumps”. I was referred to orthopedic pain physician by my occupational health clinic. I am a personal acquaintance of this ortho pain doc and thought he would be open to my recent discovery. I asked him to palpate the area with a lubricant as I read in one of your articles. I also had a coworker use an ultrasound to locate and mark those areas with a surgical marker for the physician’s convenience. Nonetheless, he gave a single poke and said “it’s probably just a lipoma” and sent me on my way for an MRI. He’s a good physician and I trust him. However, as I suspected, he deemed the injury to be of soft tissue and my spinal anatomy demonstrated only moderate disc herniation of L4-S1 consistent with aging. I agreed to a steroid injection and nerve block that provided minimal relief for 48 hrs. I am resorting to cosmetic liposuction “360” in hopes of a solution.** Furthermore, my sister and mother both have the same pain complaints and I was able to palpate similar “lumps” in the same areas…possible genetic component?
Note: I am so thankful for your publication “Historical Review of Studies on Sacroiliac Fatty Nodules (Recently Termed “Back Mice”) as a Potential Cause of Low Back Pain” which I shared with the Interventional Radiologists I work with.
I am in my final semester as an MSN-FNP student and I look forward to investigating back mice, tremendously, and providing service where patients feel “heard.” I have proposed this topic for my capstone project and will be requesting to make my presentation to a group of medical professionals at the acute care facility where I work for my final grade.
Can you advise? Where do you suggest I seek a consultation for this issue?
Dr. Parera,
Furthermore, I read your reply to Malcom, which answers part of my question.
Can these injections be performed by palpation with out imaging?
Dear Tiffany,
Yes, the intra-nodule local anesthetic injections can be done without imaging.
Saludos,
Marta
Dear Tiffany,
Thanks for your message, and sharing your story within the blog.
Unfortunately, I do not know a “specific” physician in US with who you could seek consultation. Not even here in Spain… yet.
I am really happy to listen that you look forward to investigate back mice, we still need a lot of questions to answer, and the webpage is there to share the information so we move forward with it.
Best wishes,
Marta
I would like to find someone in southeast Louisiana that can help me with back mice. I’ve had this for 10 years. It doesn’t show up on mri or ultrasound.
I have been robbed of $1000 so far, every one I visit is another $100 and none of them know what they are doing.
Do these “back mice” get progressively worse? Im 23 and have been having right side lumbar pain when standing/walking for long periods of time for the last year or two but over the summer it started to get worse and these last few weeks its gotten to where anything over 15-20 minutes on my feet is unbearable. While massaging the are last week I found a strange lump deep under in there just above the crest and also found one on me left side in the same spot although I’ve never had any issues with that side. I am planning on seeing the doctor this week but am worried about what route he will want to take. I just want to be pain free and be able to live my life like a normal guy!
Dear Andrew,
Back mice (fibro-fatty lumps in the lower back) can be a common finding in many people. Often they are not painful under palpation. An often they appear in both sides in the lower back.
We suspect that the back mice is causing the pain by cluneal nerve irritation if while pressing the nodule the back pain is triggered.
As far as I know, indeed the back mice can become progressively worse.
Saludos,
Marta
Thanks for your reply! I went to my doctor and he pressed around on them and said they could not be the source of my back pain (go figure!) He firmly believes its a muscular issue but I don’t see how a muscle strain would slowly get worse over the course of a couple years, those are usually worse in the beginning and slowly get better or stay the same. He did agree to order an MRI that I am having on Friday. Hopefully they can see something but if not I am almost certain its this lump that is causing the pain! I only get it when standing up or walking so I don’t know how to prove to them this is the issue.
Andrew, I’ve had painful bi lateral mice for two decades. I had a disk injury before they appeared and recently had spine surgery, decompression. I still have the pain in my lumps. My GP was clueless. I’m going to keep trying to find help. I’m in Arizona. If you find a surgeon who can help you let us know. I’ll do likewise. Mary Anna
I am also in Arizona and struggling to find a doctor willing to remove mine. If you find anyone please let me know!
After suffering a traumatic fall; I too have fallen pray to the dreaded back mouse. I even flew to the Mayo Clinic in Arizona… I saw a neurosurgeon there and their hernia specialist. Both said my MRI was clear of hernias and told me they will NOT operate on me. Despite having these lumps on my back.
I even had a lipoma surgeon do a small incision and he confirmed I had hernia fat that had torn through the fascia.
Even after explaining all of these medical findings to the Doctors at the may clinic; they still refused. Beyond frustrating. I’m now talking to a hernia specialist in Brisbane Australia.
My doctor just told me they only come up on xrays not MRIs
I have had it 10 years. Mine are worse every year.
Did you get an ultrasound examination?
I am so glad I found this page!! I have been suffering since last September with “back mice” in my lower left back. I have had an ultrasound and an MRI. I was told by 2 surgeons – one general and one neurological that surgery wasn’t a good option. Possible injections, physical therapy and accupuncture.
I have been doing PT and acupuncture for 2 months and the pain is getting worse. I was also told to “take it easy.” I am a 58 year old single woman who lives by herself and cannot “take it easy” as they say. I can barely bend over to feed my cats anymore.
I scheduled another appointment with the neurological surgeon to at least start injections for the pain. I am going to ask for a referral to a surgeon who will remove this ASAP. I would love to find someone who knows how to do this and has done several so I will see what he says and get back to all of you. I wonder how much fascia damage I have as I may have injured it last fall. I went on a long cross country 11,000 mile car trip over 2-1/2 pos where it became progressively worse. Now as I am more stationery it comes and goes but when it does come its horrendously painful. I ice and heat and take OTC pain relief. I cannot believe more attention isn’t paid to this issue. How many are suffering from this!????
I have been diagnosed with hypermobile Ehlers Danlos and now Dercum’s Disease this week. Is the mouse similar in structure to the other painful lipomas I have around my body (ribs, thighs, upper arms, hips). I’m hoping I can get someone to just ultrasound my entire body 😂
I’m having at least 4 back mice on my lower back. I’m wondering if that’s causing my sciatic pain? Also I have a swollen lymph node in my left groin. Is this the reason for the swollen lymph node? It’s constant pain and I can see them. What I’m the world causes these?
Hi Laura,
The best way to be sure that the painful nodes are back mice is performing an ultrasound by somebody that knows about this subject. Swollen lymph nodes should be investigated a part and, as far as I know, they are not associated with the back mice in common cases.
Regards,
Marta
Hi all .I’ve had the same Lower back pain for over 30 years .It would come and go over time .
In the last year it has given me constant pain .
I have had all the treatments massage ,osteo chiro you name it .Pain doesn’t disappear.
I’m actually struggling to work as it’s affecting my life tremendously.
I had a CT scan done six months ago and nothing showed up .Two weeks ago my doctor sent me for an ultrasound and I was diagnosed with a lipoma .
I’m booked in for surgery next week to have it removed by a general surgeon.I will have to have a general anaesthetic for it .
Hoping that removes all that nerve pain I’ve been experiencing.
Even my surgeon was adamant that lipomas don’t cause pain .For some reason they refuse to recognise that these back mice cause so much pain .Will keep you informed on my pain post surgery .
Dear Mary,
I hope that you get better. The surgeon should know about the cluneal nerves prior to surgery.
Regards,
Marta
Hour did surgery go?
Hey Mary, did you end up having surgery? Did it work reducing your back pain?
Glad to find this site and your research. I am a pain management anesthesiologist in the Kansas City, Kansas area and have been specifically treating these for the last 10 years when I first identified these as a source of pain in my patient population. I didn’t know until relatively recently about the names for it. My treatment protocol which seems to work for my patients is similar to what I have read recently, i.e., 1) inject with 10cc of local/steroid under ultrasound guidance into and around the lipoma/fascial layer several times as needed, and 2) if unsuccessful or not long lasting, refer to a local plastic surgeon for excision. This has been very successful with, I would estimate, ~90% favorable outcomes. The hard part was finding a plastic surgeon that was willing to do this. Most said they didn’t know what I was talking about and couldn’t help them.
Thanks for maintaining this website and info.
Daniel Bruning, M.D.
Dear Dr Bruning,
Thanks for you message. It is good to know doctors that may treat patients suffering form this condition in Uniated States. Since many times they ask about it on this website.
Regards,
Marta
I am a desperate 50 year old woman in agonizing pain that needs a plastic surgeon that has had success removing these, asap. I’ll go anywhere. Please help! Giaevitah@gmail.com 4802581392
Dear Gia,
I’m sorry to hear about your pain. To diagnose and alleviate it, I recommend two steps:
Anesthetic blocks: Request any doctor to perform these blocks on the painful back mice area. It can help provide temporary pain relief while serving as a diagnostic tool. If the pain diminishes, even temporarily, it indicates its origin in that region. This procedure is commonly performed by doctors. The blocks also are used to treat pain, and can be repeated several times.
Ultrasound: Prioritize getting an ultrasound of the area before considering surgical removal of fatty tissue.
Please consult a medical professional who can assess your situation and provide personalized advice.
Wishing you relief and a speedy recovery.
Marta Cañis Parera
Hello Dr Bruning,
I am suffering terribly from back mice that have progressively gotten worse and worse and noone has any idea what I’m talking about in Cincinnati. Pain doc, ortho spine surgeon PA’s and the NP gate keeper at University Cincinnati Neuroscience. I hav various other spine issues and had cervical fusion last year. A radiologist at UC may have also noted a spinal epidural lipoma but I can’t get an answer for that either. Can you recommend anything that i can do to resolve this troublesome situation??
Thank you, Sarah
Hey Everyone,
Just a follow up to my condition. I’ve had these lumps for awhile and had been suffering for sometime. Nothing would show up on any scans. I’ve had 3 MRI’s, a contrast CT scan, nuclear medicine bone scan, Xrays, 2 Ultrasounds…. and none of them showed up what these lumps on my back were.
Anyways, long story short I managed to find an amazing plastic surgeon here in Vancouver Canada; who agreed to perform surgery. I went under general anesthesia and surgery lasted 2 hours. He was very thorough. He said he found 2 tears in the fascia (one on each side). He removed a total of 100 grams of ruptured fat. I have pictures of the fat he removed.
I’m now 2 weeks post operation and I’m feeling significantly better. I’m not 100% better, but I’d say maybe 80-90% better.
If you’re suffering as I had been… please talk to a plastic surgeon.
Cheers,
Kel
Hi Kelly,
Thanks a lot for your contribution to this blog with your experience.
How long was recovery from getting this removed?
Who was your doctor?
Does anybody know any doctors in the USA that treat back mice? Nobody seems to pay much attention or know anything aobut them when I inquire.
Actually, I am about ready to go out of country as well! But if I could stay in the USA it would be more convenient.
If I have to I will go outside the US, but it would be more convenient to stay inside the US. Thanks, Randy
Had a deep Episacral Lipoma (5cm plus long upon palpating) removed today by Plastic Surgeon. Just recently (last several months) causing more referred pain, over to hip, in front right thigh, lower lumbar region when standing. Been present for 5+ years. It took surgeon a while to dig it out. He was able to get through some muscle without cutting which I’m grateful for. He said it was tucked pretty well into some nerves.
After freezing abated, pains which could be felt through ibuprofen and Naproxen dosing yesterday not present now 7 hours after surgery. Better walking range of motion after freezing wore off, no restriction in gait, no pain or weakness.
My nurse took a picture of the excised lipoma tissue if there’s a way to submit it… thanks.
Dear Jeffrey, thank you very much for sharing this information through your blog. I hope that your pain improves soon. However, I do have a few questions:
Did you receive a previous diagnosis through ultrasound and local anesthetic block of the cluneal nerves?
Was the surgeon knowledgeable about subfascial fat herniation and cluneal nerve entrapment?
Could you please send us a photo to the email contact@backmice.info? Do you have photos of the surgical removal itself? They would be very informative. Also, a photo of the scar would be appreciated.
I wish you a speedy recovery.
Marta
Hi Marta
Most of my pre op symptoms have disappeared since the surgery a week ago.
Post op I’m sore from local swelling where incision was made.
My nurse visited today to check stitches and change dressing. I forgot to ask her to take a picture of the surgical entry. She’s back Thursday or Friday and will try to remember to ask then…
Regrettably she didn’t take a picture of the lipoma during procedure, but I can describe it to you. It was only partially sheathed by the time it was extracted as it couldn’t be readily removed intact because of nerves in area and depth of lipoma. Dr Wyatt was aware of the cruneal nerve and that pressure from the lipoma could be causing the hip pain… the lipoma was essentially a partially sheathed grouping of beads they looked like, darker than I expected, like a dark honey colour, closer to dark golden than the yellow I was expecting. There wasn’t despite the depth, a lot of blood. He closed using three sets of four stitches across three layers as he described it.
I’m going to ask if he wrote a post procedural report and if he did or made notes I’ll try to get a copy.
Anyway, I hope some of that helps.
As of now, my pain is mostly from sitting where there is pressure on the wound area. It’s getting better.
Sorry lastly we discussed the idea of a fat herniating precipitated by a facial tear from a fall on stairs several years ago… Best…
Dear Jeffry,
Thank you for your contribution to the blog. If you are willing, please send the photos of the excised fat and the scar to contac@backmice.info. We appreciate your kind contribution.
Please keep us updated on your progress. We hope to see further improvement from you as the days go by.
Additionally, we have a request. We are currently compiling a list of medical doctors who are knowledgeable about the back mice issue. Could you ask your doctor if he would be interested in providing his contact information? This way, we can refer future patients in the vicinity to him.
Best regards,
Marta
Please please please provide me your doctors name thank you!
Hey can you please email me the pictures…I want to have this surgery and want to go to the doctor with proof…also where did you get the surgery done? Deontelomax@gmail.com or text me 3127217123
Who was your doctor??
Are you abel to share the name of your doctor?
Marta,
I emailed post op lipoma pics.
Jeffrey
Thank you!
Hi Jeffrey,
Thank you for sending us the photos. Please provide me with an update on how you are progressing with your symptoms. I sincerely hope that the surgery has been beneficial for you. Could you kindly let me know the name of the doctor who performed the surgery? Perhaps they would be interested in receiving patient referrals from me. Additionally, I’m curious to know the cost of the procedure. You can send a private email to contact@backmice.info for that.
Looking forward to hearing from you.
Best regards,
Marta Cañis Parera
Hi Marta,
Soo many are suffering. Please let us know the doctors who are willing/can help.
Thank you!!!
Hey Faye,
I’m at a bit of a dead-end when it comes to finding docs familiar with the “back mice phenomenon.” It’s quite niche in the medical world at the moment. The concept of fibrofatty tissue dysfunction being a pain source isn’t widely acknowledged these days, even with numerous historical publications from doctors trying to raise awareness about it.
I launched a webpage to spread the word and share my insights. We’re making strides, but there’s still much ground to cover. On a positive note, any doc can conduct a diagnostic test using a local anesthetic intranodular block to determine if pain originates from the “back mouse” region. I’d like to remind you that repeated local anesthetic injections and multiple hypodermic dry needling have been employed as treatments for this pain. Additionally, requesting an ultrasound to confirm the back mice diagnosis is straightforward and can be done by any radiologist. If it comes down to surgically removing a nodule, most general or plastic surgeons should be equipped to handle it. They just need to be briefed about the cluneal nerves and the optimal procedure to minimize scarring.
I wish I could provide a list of specialists now. Fingers crossed more doctors become familiar with this in the near future!
Reach out if you have further queries!
Marta Cañis Parera
Thank you for the reply. I went to go see a highly rated plastic surgeon and he said the mice could definitely be causing pain but if not removed correctly then it could also cause more pain due to the cluneal nerves being there. That’s his worry. He suggested I get an ultrasound and it did not show anything. The ultrasound said it may not have shown up if it is encapsulated. Nothing is showing up on MRIs or ultrasounds and I’m frustrated. The doctors and technicians all agree something is there. They can feel it when palpated. Also was thinking of seeing a neurosurgeon if he’s nervous about nerves. Thoughts?
Dear Faye,
Did any doctor attempt a local anesthetic block in that area to see if the pain subsides? It’s a straightforward very easy diagnostic test that any doctor can perform. If blocking the cluneal nerve transmission alleviates the pain, even temporarily, it suggests that something in that area is irritating the cluneal nerves and sending pain signals to the central nervous system. This diagnostic method can sometimes be repeated to manage pain before considering surgery. If the ultrasound didn’t show any back mouse, it’s advisable to consult a specialist in superior cluneal nerve entrapment.
Hello Marta, Thank you for the insight! I have not done a local anesthetic block that I know of? I did get an injection (1% lidocaine & dexamethasone) which was injected into my illiolumbar ligament (located behind my fatty nodules) which started to alleviate some pain after 4 weeks. The pain relief did not come right away. Does this count as an anesthetic block? Typically, how long do anesthetic blocks work if they do? What kind of doctor is a superior cluneal nerve entrapment specialist? Would that be a neurosurgeon or general pain specialist?
I am trying to get a pelvis MRI with contrast done to see soft tissue for possible tear of fascia. Sorry for all of the questions, thank you for creating this board/forum!
Dear Faye,
Thank you for reaching out with your questions.
The injection you received in the iliolumbar ligament does not qualify as an anesthetic block. An anesthetic block typically targets the painful “back mouse” nodule or, at the very least, the typical point of the superior cluneal nerve above the iliac crest. This block serves as a diagnostic test initially. If the pain is due to a “back mouse” or a superior cluneal nerve entrapment, relief is typically immediate. This immediate relief acts as the diagnostic indicator. However, some patients opt for repeated blocks in that area, usually 1-4 times within a span of weeks, as a form of long-term pain relief therapy.
Regarding your MRI with contrast, I’m eager to see its results. To the best of my knowledge, I’m unaware of it being used specifically to detect fascial tearing.
In terms of specialists for superior cluneal nerve entrapment, both neurosurgeons and general pain specialists can treat this condition.
I hope this information is helpful to you. Please don’t hesitate to reach out if you have any more questions.
Warm regards,
Marta Cañis Parera
Thank you for the detailed response!
I will show your comments to my orthopedic doctor when I follow up on Wednesday. When I find out the results of the pelvis MRI I will also inform you. Very grateful I found this page!
Sincerely,
Hello Marta,
I just came back from my orthopedic doctor. He said he can inject the nodule if I wish. Is this the same thing as anesthetic injection you were speaking of? What specifically is the doctor supposed to inject for it to be considered an anesthetic? Lidocaine? cortisone? dexamethasone?
Thank you!
The technique is quite straightforward for any physician; it does not need to be a specialist. It involves injecting 2-4 ml of a local anesthetic, such as lidocaine, into the painful nodule using a needle that is 1-1.6 cm long, which is sufficient for subcutaneous lengths. If the pain disappears, this indicates that it is originating from that area, specifically from the local terminations of the cluneal nerves. Remember, some patients achieve pain relief by repeating the local anesthetic blockade several times, always targeting the most painful spot upon palpation.
Thank you Marta; I really appreciate your help. That will be my next step. Problem is I’m not always in pain. I’ll be in touch if anything new arises. I still have an appointment with plastic surgeon next week and neurosurgeon in December.
Hello Marta,
Neurosurgeon canceled my appointment as I wasnt a candidate to see him. I never got the local anesthetic blockade but the plastic surgeon said he will take them out on November 30th. Prayers appreciated! Thank you!
Buen día Marta.
Por mucho tiempo he palpado bultos en la zona sacoiliaca derecha, tengo dolor en toda la zona derecha del cuerpo, dolor en la pierna, gluteos, zona lumbar etc. Me he realizado ecografias y resonancia en la zona sacroiliaca. En la ecografía salen pequeños lipomas pero en la resonancia salen un poco mas grandes.
Mediante mi palpacíon parece haber muchos lipomas y más grandes.
Esto son las mediiciones en la resonancia
15mm AP- 23mm T
16mm T – 13mm AP
22mm T x 17.
Tengo 3 lipomas, en la zona sacroiliaca. Sin embargo me dicen que son pequeños para considerar la extirpación.
MI preguntas son:
1. El tamaño de los lipomas determina el dolor?, es decir puede un pequeño lipoma producir mucho dolor?
2. Hay una diferencia entre los examenes de ecografia y resonancia, y la palpación.
Qué tan efectivo puede ser una ecografía o resonancia en la detección de lipomas?
Hola, gracias por tu mensaje. Primero que todo, los ‘back mice’ o ratones de la espalda NO son ‘lipomas’ exactamente. Estamos investigando qué son realmente. Aunque a menudo se les ha denominado ‘lipomas episacroiliacos’, en realidad no lo son. Si hablamos de los ‘back mice’, el tamaño no tiene relación con el dolor. En nuestro modelo teórico, lo que genera dolor es cuando el tejido fibrograso que forma los ratones de la espalda se hincha y comprime los nervios periféricos cluneales (consideramos que la hinchazón es de contenido acuoso, linfa). Respondiendo a tu segunda pregunta, la mejor manera de determinar si se trata de “back mice” es mediante ecografía. Sin embargo, la persona que realice la ecografía debería estar familiarizada con la existencia de esta entidad clínica que estamos investigando. De lo contrario, no sabrá identificar lo que está viendo correctamente.
Saludos,
Marta
My back mouse removal surgery went well. It has been 2 weeks post op and the pain is pretty much gone. I am able to sit again for much longer periods of time. I still have discomfort at the incision site and hoping that heals up in a few weeks. My doctor was amazing, I recommend him and trust him for any type of plastic surgery procedure. He gave me permission to provide his name for anyone else looking for a competent and knowledgeable doctor: Dr. John Louis in Sanatoga, Pennsylvania. I am so grateful for him and appreciate this site as well. Thank you for the support Marta! You are making a difference!
I have pictures of the mice if you would like them for research.
My email is fayeromano@gmail.com
Hi, I’m in New Zealand, Auckland do you know a surgeon willing to remove my back mouse.
Also do you think ultrasound cavitation could help break down the tissue of the back mouse?
Thanks Sarah
Hi Sarah. Unfortunately, I do not know anybody I could address this to. However, before considering surgery, other options should be explored. First, an anesthetic block should be performed to confirm if the back mouse is related to the source of pain. Afterward, continue with subcutaneous dry needling on it. Sometimes, this approach may be sufficient before contemplating surgery.
Join the back mice Facebook group-I saw someone recently from New Zealand asking the same question.
How are you feeling now ? Did the facia repair also done part of excision ?
I experienced severe back pain. Palpitation of the lump exasperated the pain. Pain, burning and numbness radiating down glutes around to front of thigh and groin. Numbness resolved after 5-6 weeks, but pain and burning return with light exercise.
Surgical excision seems like the best option. But I am wondering what type of surgeon?
I completely understand your concern and the pain you are experiencing. It is essential to perform an accurate diagnosis before proceeding with any treatment. Ultrasound is a key tool that complements palpation in detecting back mice, as it allows visualization of the internal structure that may be causing the issue.
Many patients have found relief by repeating anesthetic blockages in the affected area, thus managing the pain without the need for surgery. This therapeutic option can be repeated several times, and in many cases, can avoid surgical intervention. Superior cluenal blockage is another option.
Surgery should only be considered when it is confirmed that the persistent pain is directly caused by the fibrous fatty nodule, especially if it is causing extreme compression. In these circumstances, it is crucial that the procedure be performed by a surgeon with specific experience in this type of intervention to minimize possible complications.
I hope this information helps you to work with your medical team to find the best solution for your case.
Hi, I emphasize that before considering surgery, the best approach to addressing the back mice issue is a thorough diagnostic evaluation. This should include palpation, ultrasound, and a local anesthetic block. If the pain diminishes after the block, it may indicate that the fibrofatty nodule is indeed the source of the pain.
If the local anesthetic block provides temporary relief (even if only for a few hours), it should be repeated at least three more times over the course of several days. This can potentially lead to longer-lasting relief. In some cases, the anesthetic may need to be applied to the entire area surrounding the nodules, as everything may be swollen, and the needling helps to decompress the area.
Subcutaneous dry needling is also an effective technique to relieve pain from this edematous fibrofatty tissue.
Marta Cañis Parera
Are back mice associated with lipedema?
Hello Marta, my name is Tereza and I have been going through this pain for almost 2 years now. The back mice appeared after I had my baby in January of 2023. It was a very traumatic experience and I haven’t seem to be able to heal back to normal since. I have tried everything and the doctors, chiropractors, physical therapists have all been clueless to the issue or down played its significance. This was in Kansas, USA but I have recently moved to Poland and started my first year of medical school. As a medical student I am very intrigued by what is happening especially as I’m learning those structures but I am at a loss for how I can get the help I need., especially as my symptoms worsen as I sit and study. This pain is getting too much to bear, especially on days when I have a full school load as well as a needy toddler. There is no comfortable sleeping position and I lose a lot of sleep trying to ignore the pain. What kind of specialist do you recommend me to go to? Is there any way I can help your study? I am very interested in research and would love to help in any way I can. Thank you and I look forward to hearing from you.
Dear Tereza, I will answer through an email.
Thank sounds great and very much appreciated. I sent an email prior to the contact email listed and I’m not sure if you can see that on your end or not but here is my email just Incase.
Terezazardoz@gmail.com
Hello Teresa,
I’m sorry for taking so long to reply. The issue of dysfunction in fibro-fatty tissue or fatty fascia is a forgotten topic in medicine. We have created a foundation to advance knowledge about this tissue (which is often mistakenly discarded in dissection rooms), to understand its basic structure, and to gain a better understanding of its dysfunctions. The foundation’s website is http://www.fasciopathiesresearchfoundation.org.
The phenomenon of back mice is one of many pathophysiological phenomena that fibro-fatty tissue can present.
Additionally, we have a private clinic near Barcelona where we can assess you and treat your pain. If you are interested, you could come and try it out. The ultrasound and treatment cost €60. Here is the link to our website, where you can find testimonials: http://www.mdfascialtherapy.com, and the link to the clinic: https://www.doctoralia.es/clinicas/caf-vendrell.
We use the “teasing” technique developed by Dr. Copeman. Without any medication, we achieve excellent results. This technique involves using a sterile subcutaneous needle. It doesn’t hurt, but it can be a bit uncomfortable, and some bruising may occur.
I hope this information is helpful, and if you decide to visit, it will be a pleasure to assist you.
Best regards!